Fearless
It was Aug. 25, 2018, just another scorching San Antonio summer day, when an American bulldog attacked 3-year-old Brooke Brady, inflicting horrific injuries on the tiny, blond-haired girl. Eleven days later, on Sept. 5, Brooke walked out of University Hospital, bandaged but smiling, and wearing a pink tutu. What happened between those two dates is an extraordinary story of one patient’s untiring courage and the incredible expertise of a team of UT Health San Antonio physicians and caregivers.
It’s a remarkable story yet, in a way, remarkably ordinary. It’s one story out of so many.
Brooke’s dad, Justin Brady, was in Washington, D.C., on business, and her mom, Kim, was on a weekend getaway with friends in Port Aransas that sultry Saturday. Brooke and her sister, Riley, 5, were in the care of a sitter when the attack occurred.
Brooke was rushed by ambulance to University Hospital. She had extensive crush injuries to the torso and major lacerations. Her left lung was punctured and filled with blood. Eight ribs were fractured. That day, Susannah Nicholson, M.D., the on-call trauma surgeon, took Brooke to surgery for bleeding control. It was the first of four surgeries, performed every other day. Trauma surgeons Lillian Liao, M.D., M.P.H., and Deb Mueller, M.D., and plastic surgeon Amita Shah, M.D., also treated Brooke. She was intubated, cared for in the pediatric intensive care unit and was heavily sedated the first three days.
Her terrified parents rushed home to San Antonio. “I mean, seeing your little 3-year-old, fragile, clumsy daughter with tubes coming out all over her body, it was just … words can’t describe that feeling,” Kim Brady said, fighting back tears. It was only after speaking to one of the doctors who calmly explained her treatment and reassured them, she added, that she felt she could breathe.

‘Calm and cooperative’
Dr. Liao is a clinical associate professor at UT Health San Antonio and pediatric trauma and burn director at University Hospital. The surgeon remembers Brooke as exceptionally strong.
Most 3-year-olds, Dr. Liao said, “have a bit of stranger anxiety. Brooke never had that. She was very cooperative from the very beginning when she was incredibly sick in the pediatric ICU. She was unlike most of the other children we treat in that she was so calm and cooperative and, really, super-resilient.
“At some point during a child’s illness,” she added, “we’ll see what a mom would call a ‘meltdown.’ And Brooke never really had that. She was really a super-sweet child to care for.”
Her parents described Brooke as tough, stubborn, headstrong and independent. “I think that came across during her stay” in the hospital, Justin Brady said.
Dr. Liao applied a different term. “With Brooke, I think a good word to use would be fearless.”
Caring for the whole person
University Hospital is the only Level 1 Pediatric Trauma Center in South Texas. UT Health San Antonio trauma surgeons provide the highest level of care for injured children in partnership with the hospital. The approach is multidisciplinary, Dr. Liao emphasized. Surgeons, pediatricians, residents, psychiatrists, advanced practice nurses, support staff such as Child Life specialists and the physical therapy team care for the entire person, not just the physical injuries.
“We realize that while there are visible wounds that we need to treat, there are these invisible wounds as well,” she said. “That’s where the pediatric psychiatry team comes in.”

The first doctor that Brooke communicated with was a psychiatrist, Kim Brady said. He used play therapy and props to elicit dialogue and help Brooke deal with the understandable fear and stress, and haunting memories of
the attack.
With each passing day in the hospital, Kim and Justin Brady said, they grew more impressed with the caregivers’ medical expertise, compassion and communication skills.
“At 5 or 6 a.m. every day,” Kim Brady said, “I’d get awakened by the resident, just to give me a play-by-play of what’s happening, what her numbers were from the night and our agenda for the day. And the nurses were awesome. We always knew what was happening, what Brooke’s schedule for the day included.”
When something like this happens, she said, it’s difficult trusting someone to treat your child.
“But after the first meeting with Dr. Liao, I was like, ‘I don’t want anybody else to touch her.’ She just gave us so much information, so clearly, and in such a nonchalant way, like, it’s going to be OK. It wasn’t, ‘Oh don’t worry, there’s nothing to worry about,’ because it was something to worry about. It was her compassion and the way she explained it.”
“She actually thanked us,” Justin Brady said. “That last day she thanked us for allowing her to do her job. She’s just a strong, focused woman and doctor.”

A fearless future
Brooke, who turned 4 years old on Jan. 8, is back in her San Antonio preschool. She goes to physical and occupational therapy each week, and still sees Dr. Shah, the plastic surgeon, for scar management. She’s still mentally processing and working through issues, Kim Brady said, but all things considered, it’s a remarkable outcome.
“From what we saw to what we have now, in Brooke, is just incredible,” Justin Brady said. “We can’t believe it. She’s a little girl again, which is all we wanted. She has scars and stuff she’s going to have to go through, but she’s Brooke again.”
And one more thing, Kim added. Brooke has decided she wants to be a doctor when she grows up so she can help people in the same way her doctors helped her.
Acting sick

“How are you doing today?” the doctor asks cheerfully as she shakes hands with a new patient, a 55-year-old woman named Karen who smiles broadly. “Well, I’m OK right now,” says Karen, seated next to an exam table.
“So what brings you in?” the doctor asks, glancing at a chart.
“I’ve been having this awful pain in the side of my stomach,” Karen says.
And so begins another routine medical exam in a routine setting.
Except it isn’t. The “doctor” is actually a second-year medical student in the Joe R. and Teresa Lozano Long School of Medicine, and the patient is a carefully trained actor playing a part.
The encounter in the H-E-B Clinical Skills Center is part of the standardized patient program. The center’s director, Diane Ferguson, B.S.N., RN, explained that the standardized patient-student encounter is a creative teaching approach and an important component in medical education.
“We train and assess health care students on clinical skills primarily by using human simulation,” Ferguson said. “So we give [the standardized patients, called SPs] a script, a clinical case.”
Ferguson, who developed the standardized patient program at UT Health San Antonio in 1995 and has directed the Clinical Skills Center since 2005, said the encounters help students learn physical exam techniques, how to interview a patient and take a medical history and, importantly, how to communicate effectively, including when delivering bad news.
Employing SPs, she said, especially benefits students. A real patient couldn’t or wouldn’t tolerate repeated encounters with students. And using SPs, who all exhibit the same symptoms, have the same history and answer the questions the same way, allows for a better skills assessment.
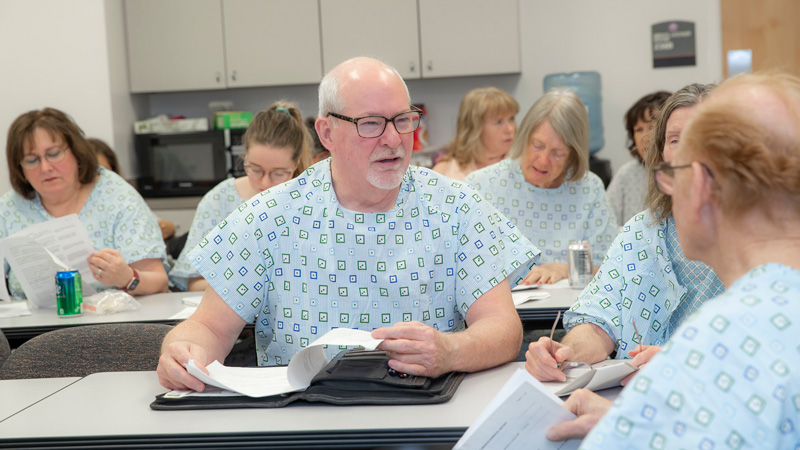
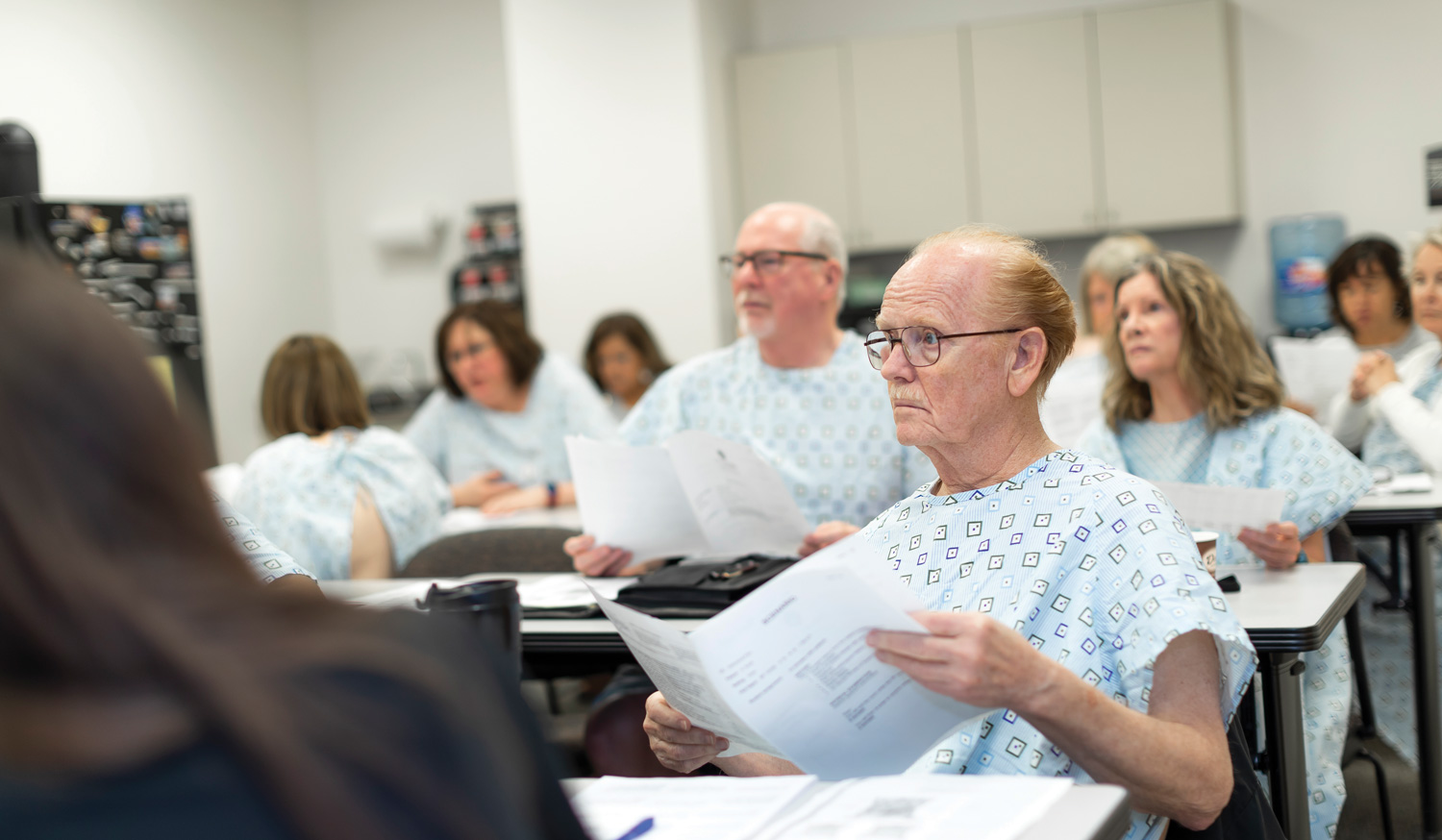
At a recent training session, standardized patient educator Kenton H. Coker Jr. hands out a case summary and script to some 20, mostly middle-aged, SPs in preparation for encounters with medical students. All the SPs will assume the identity of a patient experiencing abdominal pain. They will all memorize identical answers to anticipated history questions such as onset of the pain, duration, location, severity and associated symptoms. Additionally, the SPs are trained to recognize the correct techniques of the expected physical examination for that case.
“Every case has a demographic that we try to match if we can,” he said. “So if it needs to be a 55- to 65-year-old male, then we’ll only send out a request to that group of SPs. And each case has a specific training.”
Coker explains the objectives to the SPs, reviews the symptoms and patient history, and describes what the physical exam will entail. He reminds the SPs of the importance placed on the students’ communication skills and answers questions on how to evaluate the students based on a checklist.
There are around 75 SPs, all of whom are hourly employees of UT Health San Antonio.
One of them, Janie, has been an SP for over a decade and finds the experience rewarding.
“I really enjoy helping them become doctors,” she said. “And they find it beneficial to get the patient’s point of view. They’re grateful for what we do. Patient interaction is very important. The interpersonal skills are key. I always tell them that the better the communication is, the better their practice will be. It’s about using the right language so the patient understands and establishes trust. It’s not just about the exam.”
The encounters are serious, but there can be light moments.
“Once a student was auscultating [listening through a stethoscope] to my carotids,” Janie recalled. “He forgot to tell me that I could breathe normally again. And as a patient, sometimes you don’t know you can breathe again if the doctor doesn’t say so. So I was holding my breath until he finally noticed and said, ‘Oh I’m sorry! You can breathe again!’”

A typical encounter between an SP and medical student lasts 13 to 15 minutes, which includes the interview and physical exam. The SP then completes the checklist followed by a dialogue with the student about what went well, what the student may have failed to ask and ways to improve.
“I thought you were very thorough on your history,” Janie tells a student after their encounter. “And you had good eye contact and you smiled. That relaxes the patient.”
Time management is emphasized, which forces the students to focus on the symptoms and on interview techniques that will elicit the most information.
Medical student Alia Hemeida said the encounters are valuable.
“It’s a real application of what we’re learning so that by the time we get to a hospital setting in the third year [of medical school], we’re comfortable with patient interactions and conducting these interviews and physical exams with real patients,” she said. “It’s a safe setting for us to incorporate what we’ve learned in the classroom and start critical thinking in preparation for third year.”
Hemeida said the SP encounters are especially useful for learning how to discuss sensitive personal health issues—incontinence or sexual history, for example—with patients.
Ferguson, the skills center director, said the standardized patient program serves medical students in all four years and medical residents, as well as students from the health professions, dentistry and nursing, and pharmacy students from the University of the Incarnate Word.
She described the program as “a bridge between health care education and patient care where learning occurs in a safe environment, which allows for honest feedback that students cannot obtain elsewhere. Who better to give future providers pointers on establishing patient connections than human patients?”
Dementia
By Joe Michael Feist
Stabbing pains shot through my feet with every step, every turn. My vision was chalky and distorted. I ran into objects, couldn’t pick up a fork or knife without a struggle, and heard nothing but a god-awful, buzzing white noise. The small apartment was vaguely familiar yet foreign. Disoriented and confused, I kept trying to complete simple tasks I had been assigned, but couldn’t even remember the instructions. I felt slightly stupid and strangely lost inside what used to be my body. And under my breath, or so I thought, I cursed my predicament quite freely.
Most of all, for six excruciating minutes, I just wanted it to be over.

On this sunny spring day, I felt fine, but in a matter of minutes was about to find out what it would be like to lose my mind. The Virtual Dementia Tour is a controlled simulation of dementia symptoms and part of the overall Caring for the Caregivers program run by the School of Nursing. The tour aims to give caregivers a greater understanding of dementia and an enhanced sense of empathy for those struggling with it.
Dementia is the torturous unraveling of memory and brain function. It occurs most often in those of an advanced age, and so it’s often accompanied by other symptoms such as vision and hearing loss, neuropathy—which causes numbness or weakness in the arms or legs—and loss of dexterity. Because of the cognitive decline associated with the disease, those with dementia are often unable to communicate or explain their feelings and behaviors.
It can be a nightmare for caregivers as well, most of whom are family members with little or no training or understanding of the illness—or how to cope with an uncommunicative and seemingly uncooperative patient.
The Virtual Dementia Tour, developed by Atlanta-based Second Wind Dreams and licensed to UT Health San Antonio, is meant to give caregivers “a glimpse into the world of dementia,” said Deborah James, M.S.N., RN, a clinical assistant professor in the School of Nursing and director of the dementia tour. And, she added, a better understanding of the challenges dementia patients face can only lead to better caregiving.
This is especially critical in light of some startling facts. Age is the greatest risk factor for developing dementia, and the number of Americans over 65 is expected to double by 2060. In Texas, according to the Department of State Health Services, a new person develops Alzheimer’s disease every 65 seconds, and current projections indicate that this rate will increase to one new case every 33 seconds by 2050.
Alzheimer’s disease, the most common form of dementia, affects an estimated 5.7 million people in the U.S.; 380,000 are Texans. The disease disproportionately affects women, African Americans and Hispanics.

For the tour, which lasts only six minutes, I was outfitted with inserts in my shoes that have probes that dig into the feet. “That’s to simulate neuropathy or diabetic neuropathy, like pins and needles in your feet,” James explained. Then a padded glove was placed on my dominant hand to impede dexterity. Thick glasses distorted my vision and simulated glaucoma and other vision problems. Headphones with white noise caused hearing loss and added to the general confusion.
Uncomfortable and a bit bewildered, I was given five simple tasks, which I was to perform in a room furnished like a small apartment. But like many who take the tour, the white noise and the disorientation meant that I didn’t clearly understand the verbal instructions or recall them later. I was told to “put the coffee in the refrigerator,” but only heard the words “coffee” and “refrigerator.” I was asked to “buckle the belt,” but only heard “belt.” Of the tasks assigned, I completed none.
“All of the things being simulated are very common in those with dementia or those with Alzheimer’s,” James said.
My tour was a marathon of frustration, pain, embarrassment and defeat. I fearfully thought, “If this is what dementia is like, God spare me.” That emotion is common, according to the Centers for Disease Control and Prevention, which found that Americans fear losing their mental functions twice as much as they fear losing their physical abilities.
After the tours, which are closely monitored, James debriefs the participants so that they more fully understand what transpired and how it might relate to their caregiving.
The experience, the sudden realization of what dementia feels like, can be life changing for the caregiver. And raw emotions sometimes overwhelm the tour participant, James explained.
“One man said, ‘I feel so ashamed,’” she recalled. “He said, ‘I try to protect my wife, but I never realized that it hurts so bad just to get your damn shoes on. I didn’t know she was in that kind of discomfort. And I never thought that she couldn’t hear me.’”
Like other caregivers, the man thought his wife simply didn’t want to cooperate.
Sheran Rivette, who works part time in the Caring for the Caregiver program, was the full-time caregiver for her husband, who had Alzheimer’s disease, for six years before his death in February 2017. She now cares one day a week for a man with Alzheimer’s, giving his wife a much-needed respite.
She recently experienced the dementia tour, but, for her late husband’s sake, wishes she had had the chance to do it years ago.
“At first, after doing the tour,” she said, “I had sadness because I had not been as sensitive in understanding his conditions and his actions as I could have been. Should have been.” Her voice trailed off. “Wish I had been,” she added softly.
Almost worse than the disease itself are the moments of clarity, in which the person with dementia realizes how much they’ve lost.
“I think the person is disappointed when they can’t complete simple tasks,” Rivette said. “I think they’re embarrassed because they feel foolish, they feel stupid. My husband often said, ‘I’m just stupid. I don’t know anything.’”
Now, she added, with the man she cares for weekly, she’s more patient, more tolerant, more willing to try different approaches to break through the fog of the disease.
“I would encourage every caregiver to take this tour,” Rivette said. “To empathize is different than to sympathize. I believe empathy is huge. We need to put ourselves in other people’s shoes.”
By far, family members provide most of the care for loved ones with dementia or Alzheimer’s disease, said nursing professor Carole White, Ph.D., RN, who directs the Caring for the Caregiver program. In 2017, an estimated 15 million Americans provided 18 billion hours of unpaid care for family members and friends with Alzheimer’s and other dementias.

Often, Dr. White said, it comes at “great personal cost to their physical health, their emotional health, their social and financial health.”
That’s why the comprehensive Caring for the Caregiver program that offers education, skills training, research and community engagement is so needed, she said, especially in light of the coming “tsunami” of people with Alzheimer’s disease and other dementias.
After my dementia tour, as I massaged my aching feet, regained my balance, was told how much I swore and was reminded of how I didn’t really do the things I was asked to do, James added a sobering shot of reality.
“Remember,” she said. “This was only six minutes of your time. It’s every minute of some people’s time.”
The School of Nursing and the Glenn Biggs Institute for Alzheimer’s and Neurodegenerative Diseases work together to support the health and well-being of people with dementia and their family members. To learn more about the Caring for the Caregiver program and the Virtual Dementia Tour, visit UTcaregivers.org, call (210) 450-8487 or email masoud@uthscsa.edu.
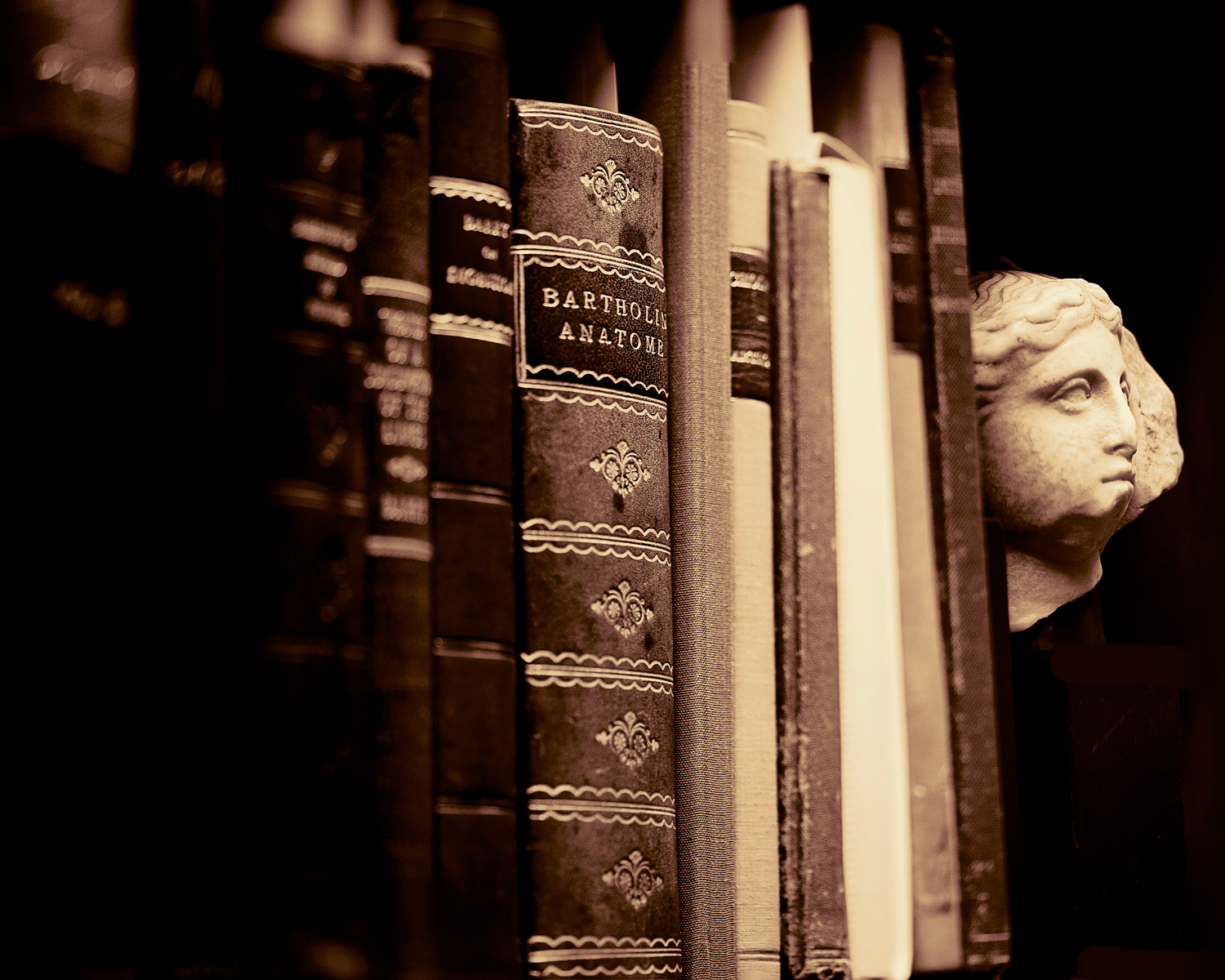
Treasures of the P.I. Nixon Library
By Joe Michael Feist
Tucked away on the fifth floor of the Dolph Briscoe Jr. Library, the collective wisdom of thousands of years of medical exploration lies waiting to be discovered anew.
The treasures of the P.I. Nixon Medical Historical Library reveal the evolution of medicine and the methodical untangling of many a mystery. Included are some of the rarest and most beautiful medical texts ever created.
The Nixon library, a part of the overall Briscoe library, is named for Patrick Ireland Nixon, an early 20th-century San Antonio physician and book collector who in 1919 founded the Bexar County Medical Library Association. Through the years, with Dr. Nixon overseeing the library and purchasing many books himself, the association acquired thousands of priceless works on medicine and health. In 1970, some 6,000 books from the association were donated to UT Health San Antonio, forming the core of the Nixon library.
“Any student at UT Health San Antonio can benefit from the early books in health care, which are basically the origin of the fields they’re going into,” said Andrea Schorr, the Briscoe library’s head of resource management. “It gives them perspective as to what has been done historically and what is happening now.”
Mellisa DeThorne, special collections assistant, said the Nixon library contains works on general medicine, most specialties, dentistry, nursing and many other aspects of health care. But the books transcend medicine, she added. “Anyone who has an appreciation for art can appreciate the books in the Nixon library, because they are works of art.”
In addition to the core collection of books, the Nixon library also includes some 200 medical devices, photographs, artifacts and other historical items.
[bgsection pex_attr_title="Here are a few gems from the Nixon collection" pex_attr_subtitle="" pex_attr_undefined="undefined" pex_attr_style="section-dark-bg" pex_attr_bgcolor="f8f1e1" pex_attr_image="" pex_attr_imageopacity="0.5" pex_attr_bgimagestyle="static" pex_attr_titlecolor="000000" pex_attr_textcolor="000000" pex_attr_height="" pex_attr_cssclass=""]
|
Milan, 1481, second edition Significance: The Latin De Medicina is the oldest book in the Nixon library collection. The work, consisting of accounts of medicine in Roman times, is the only remaining portion of a much larger encyclopedia by Celsus and is generally considered among the greatest medical classics. Worth knowing: Hippocrates used the Greek word carcinos, meaning crab or crayfish, to refer to malignant tumors. It was Celsus who translated the Greek term into the Latin cancer, also meaning crab. |
 Tables of the Skeleton and Muscles of the Human Body, by Bernhard Siegfried Albinus (1697–1770) Tables of the Skeleton and Muscles of the Human Body, by Bernhard Siegfried Albinus (1697–1770)
London, 1749 Significance: Albinus, a German anatomist, along with his artist Jan Wandelaar, is highly regarded for this work of magnificent engravings. Aiming for absolute precision and scientific accuracy, they used a unique grid pattern technique for copying the anatomical specimens. Worth knowing: The work is almost as well known for its lush, whimsical backgrounds of nature and, especially, Clara the rhinoceros. Albinus did this “in order to relieve the harshness of the figures,” Schorr said. “He decided to create the illusion of three-dimensionality in his illustrations.” |
|
Significance: Fascinating tales of Texas frontier medicine fill these two, beautifully hand-written volumes of casebooks by pioneer physician George Cupples. Dr. Cupples was a Scottish-born surgeon who moved to Texas in 1844 in the hopes the climate would revitalize his ailing wife’s health. He subsequently served as surgeon for the Texas Rangers in the Mexican War and then for the Confederate Army. The cases, which cover the period from 1850 to 1877, include detailed accounts of everything from a gunshot wound and amputation, to a penetrating knife wound to the heart, to opioid addiction, to a 60-hour labor and delivery complicated by a cervical tumor. Worth knowing: Dr. Cupples was renowned as an innovative surgeon and is believed to be the first physician in Texas to use anesthesia.
|
|
Basel, 1543, first edition Significance: The Fabrica is the rarest and most valuable book in the Nixon library. It’s also the most viewed. “It was Vesalius who first dissected a human body and described what he found in great detail, and therefore had a far better understanding of the way our bodies work than [Greek physician, surgeon and philosopher in the Roman Empire] Galen,” DeThorne said. “Vesalius is the father of modern anatomy.” Worth knowing: When it was purchased by Dr. Nixon in 1939 from Yale University for $765, it was said to be one of only 16 copies in the United States and fewer than 200 in the world. |
|
Dresden, 1583, first edition Significance: Bartisch established ophthalmology as a separate medical specialty and his Ophthalmodouleia was a landmark publication. His descriptions and illustrations of eye surgeries and the anatomy of the eyes were striking and revolutionary. Worth knowing: In German, Ophthalmodouleia was one of the first medical books to be written in the vernacular rather than Greek or Latin.
|
|
Venice, 1486 Significance: The book in the Nixon collection is one of five in an encyclopedia of medicine by the 11th-century Persian philosopher, scientist and physician Abu ‘Ali al-Husayn ibn Sina, translated as Avicenna in Latin. Canonis libri V is devoted to compound drugs. Worth knowing: Avicenna’s work attests to the fact that medicine in the Middle East at the time was often more advanced than in Europe.
|
|
London, 1667 Significance: Robert Hooke is known as a “Renaissance Man” of 17th-century England. His work in the sciences covered astronomy, physics and biology as well as medicine. Micrographia, his most important writing, documented experiments with a microscope. An artist as well as a scientist, he did all of his own illustrations. Micrographia is basically the origin of microbiology. Worth knowing: In Micrographia, Hooke coined a new scientific/medical word: “cell.”
|
|
Dr. Matthews, an ophthalmologist, was a prominent member of San Antonio’s medical community. Active in local medical organizations, he played a significant role in the establishment of the South Texas Medical Center. On the board of the San Antonio Medical Foundation and president of the Bexar County Medical Society, Dr. Matthews secured the endorsement of the Texas Medical Association for the development of a medical center and medical school in San Antonio in the 1950s. He was elected as the first president of the Friends of the P.I. Nixon Medical Historical Library in 1971.
|
|
While it undoubtedly did more harm than good, bloodletting was a popular medical treatment for a variety of ailments for centuries. By the 18th and 19th centuries, technology—in the form of the scarificator and a spring lancet such as these in the Nixon library—had replaced knives and other instruments for cutting or lancing. The brass scarificator has 13 blades and dates between 1833 and 1855. It is cocked by pulling the lever, then a button releases the blades resulting in 13 uniform quarter-inch deep cuts. A cup then suctioned the blood. Worth knowing: Massive bloodletting in his final hours probably contributed to the death of George Washington
|
[/bgsection]
The P.I. Nixon Medical Historical Library is open by appointment Monday through Friday from 8:30 a.m. to 4:30 p.m. Tours of the library, including viewings of the rare books, can also be arranged. Contact Andrea N. Schorr, 210-567-2403, Schorr@uthscsa.edu or specialcollections@uthscsa.edu.
Giving starts here
 Nicolette Speer, who graduated in August with a bachelor’s degree in nursing, believes that the concept of giving back is especially important in the health care field.
Nicolette Speer, who graduated in August with a bachelor’s degree in nursing, believes that the concept of giving back is especially important in the health care field.
“By being involved in philanthropy, you have the ability to impact more lives beyond your patient population,” she said.
The university is supported by about $70 million a year in philanthropic gifts. These contributions establish endowed professorships or chairs, fund new scholarships, support research or name a laboratory, center or school. Familiarizing students with the importance of giving back is the goal of the Student Legacy Council, said Sabrina York, director of donor and alumni relations in the Office of Institutional Advancement.
“The council is laying the foundation to keep students involved as alums,” York said. “The council’s goal is to promote awareness of philanthropy and the difference it makes to their experience as students so that when they graduate, they will be inspired to give back as alumni of their schools.”
The council, established in 2016, has 25 student members, five from each school in the university, who seek to involve fellow students.
“Whether you’re donating to a cause that you feel passionate about or giving your time volunteering, your small act of giving can make a difference in peoples’ lives,” said Speer, a member of the council.
Dear doctor, get well soon
By Joe Michael Feist
Stacy, now a practicing physician, was a resident at UT Health San Antonio when her world grew dark and frightful, shaking her as it spiraled downward. “Everything was painted black. Everything was negative. I didn’t want to do this anymore. I didn’t want to do anything,” said Stacy (not her real name), describing her descent into clinical depression. “I was changing from ‘This is great, I love this, I enjoy seeing patients,’ to ‘Why am I waking up at 4 a.m. to see this [patient] who’s just going to complain, and they don’t even know what I’m going through and they don’t care,’” she said. “I started seeing patients as a burden instead of seeing them as people I became a doctor to help.”
She was depressed, anxious, moody, had low self-esteem and seriously questioned her choices and abilities. She constantly told herself she wasn’t smart enough, that she was an impostor. Her dream of becoming a doctor became a recurring nightmare. And worst of all, Stacy added, was the feeling that she couldn’t tell a soul what she was going through. “No one can find out,” she thought. “If anyone knew, that would be the end of my career.”
Stacy felt totally alone, but in fact was far from it. In the past few years, a full-blown crisis has emerged among residents and practicing physicians suffering from burnout, depression, substance abuse and suicide.
The numbers alone are staggering.
• An estimated 56 percent of all physicians are burned out, reaching close to 70 percent in some specialties.
• One out of three physicians is suffering from clinical depression.
• Seven percent of physicians are actively abusing substances, whether illegal substances, alcohol or prescription meds.
• Seven to nine percent of physicians have had suicidal ideations in the past two months.
• An estimated 400 doctors commit suicide each year, or the equivalent of two entire classes of medical students at UT Health San Antonio. Physicians are far more likely to commit suicide than the general population. And female doctors are three times as likely to kill themselves as male doctors.
The bleak story told by the numbers means “the practice of medicine in this country is faced with a momentous challenge, perhaps even an existential crisis,” said Jon Courand, M.D., vice chair of education and training for pediatric residents and fellows, and chair of the Wellness and Resident Worklife Standing Committee at UT Health San Antonio.
Computers are not people
Dr. Courand, who has reviewed the issue extensively, pointed to several factors commonly cited as root causes of physician burnout, depression and suicide. Among these are administrative burdens, intrusion of technology, staggering patient volume and the intricacy of patient care.
“The workloads are increasing, but more than just the workload, the complexity of the patients, the acuity,” Dr. Courand said. “They’re more complex, they’re sicker and there are more of them. We’re putting a greater workload on our physicians.”
Another huge source of stress is electronic medical records (EMR), he added.
“The issue is it removes us from the patient,” Dr. Courand said. “There’s an interesting study that shows if a resident has, for example, eight patients, on average they spend about seven minutes with each patient. For those eight patients they spend less than an hour a day physically talking to people, but another four-plus hours on the EMR.
“My personal belief is we went into medicine to do one thing, and that is to take care of people, but increasingly we’re taking care of a computer screen and not people. I think that leads to disillusionment, burnout and depression,” he said. “There are a lot of people, I think, who believe the same thing.”
Years ago, most doctors worked alone in a private practice, were paid in cash, and dealt with few regulations and technology. Today, doctors across the board are under extraordinary pressure to make money, to meet “relative value unit goals,” Dr. Courand said, adding that faculty physicians in academic health institutions are not immune.
Because of “paperwork” and financial concerns, most physicians in the outpatient world spend only about 10 minutes with a patient, Dr. Courand said. “It used to be 20 minutes, then it was 15, now it’s 10.”
Straightforward cases, such as an ear infection, may only get five minutes of the physician’s time. “It’s just move ’em in, move ’em out. Patients feel that. They don’t feel that there’s that bond,” he said.
The complexity of medicine, the demands of technology and the financial pressures all affect the way doctors view their role and their self-worth. Thus the levels of burnout, depression and suicide.
“Real burnout is a low sense of personal accomplishment, emotional exhaustion and depersonalization,” Dr. Courand said. “Depersonalization is saying, I have this patient in front of me who’s suffering and may die, and I couldn’t care less. I feel nothing for this person. That’s scary. There’s a large percentage of physicians in the country who right now are either emotionally exhausted or depersonalized.”
High stress, high stakes, real expectations
For faculty and administrators at an academic health institution, one obvious way to prevent physician depression and suicide is to face the issue head on, openly and honestly, with today’s residents and students. Knowledge, and the early identification of stressors, is the key to preventing tomorrow’s depression and suicide, educators believe.
To that end, UT Health San Antonio this year hired two Ph.D. psychologists to focus on wellness with its 700 to 800 residents and fellows. The psychologists will run an interactive screening program that will send surveys to every resident and fellow asking questions about depression, suicidal ideation, burnout, substance abuse, even eating disorders.
“It’s a voluntary, completely anonymous, encrypted program that allows residents to enter into a counseling relationship with one of our providers, either anonymously through the computer or face to face,” Dr. Courand said. “And the psychologists will be promoting 45 separate wellness activities designed to promote resilience,” including everything from healthy eating to mindfulness training to quiet areas for meditation.
And it’s not just practicing physicians and residents who are dealing with these issues. Medical school students are susceptible to the same stressors.
“It’s a high-stress field,” said Thomas Matthews, M.D., clinical professor/psychiatry who spent more than nine years as associate dean for student affairs in the Joe R. & Teresa Lozano Long School of Medicine. “Even to get into medical school, you’re expected to do research, volunteer, keep your grades up. There’s so much you have to do to get in. What you’re doing is taking people who are Type A personalities or high-stress people anyway, and you’re piling things on. They come in to med school and they’re already very stressed.”
Dr. Matthews, along with Kristy Kosub, M.D., professor and director of student education for the Department of Medicine, have long worked on wellness issues in the medical school.
Just recently, Dr. Kosub said, “We have as a school really started to ramp up how we’re going to expose our students to the reality that this [burnout and depression] exists. And really making a concerted effort to make sure we’re addressing it all four years.”
Both Drs. Matthews and Kosub pointed to Veritas, the school’s student advisory group with both faculty-student and peer-to-peer advising and counseling, as a way of talking about burnout and stress.
“It’s a way for students, within their Veritas group and faculty advisers, to engage in regular meetings with various topics like burnout, so that they don’t have that feeling of isolation as they go through medical school,” Dr. Kosub said.
Other avenues toward self-awareness for students include the opportunities offered by the Center for Medical Humanities & Ethics, she said. Through electives, community service-learning projects and speakers, the center “provides the crucial element of humanism, to remind people it’s not just all about one’s medical knowledge, it’s taking care of people and taking care of yourself.”
There are many more wellness activities, lectures, social gatherings, informal talks and direct mentoring as well.
Doctors are people, too
What’s critical, faculty agree, is creating a positive environment where people feel comfortable enough to talk about stress, depression, feelings of inadequacy or being overwhelmed. And that applies not just to students, said Dr. Kosub.
“We don’t have a wellness program for existing faculty and staff,” she said. “That’s where we’re falling down. I’m hopeful that the Long School of Medicine and the university as a whole will start to build on that. The key is to make this part of the culture of the school, the residency program, the entire institution.”
At an academic health institution, Dr. Kosub added, faculty need to role-model healthy lifestyles. She noted that Stanford Medicine, in a first for a U.S. academic medical center, just hired a chief wellness officer charged with countering physician burnout and improving physicians’ sense of fulfillment and well-being.
The broader cultural issues need to be acknowledged as well.
“The stigma surrounding mental health issues and depression is rampant in all professions, including among doctors and health care workers,” said Dr. Kosub. “And it’s not just doctors. It’s a human quality of not wanting to disappoint people, not wanting to show weakness.”
As for Stacy, the former resident who walked on the edge of depression and even suicide, she found the strength and the trust in the institution that saved her.
“Finally,” she said, “I went to the program director and said, ‘I need to figure this out because I don’t want to get to the point where I can’t work anymore. It’s bad enough that I have to talk to you about it.’ And my program director actually smiled. And it was like, you’re not the first and you won’t be the last.”
Stacy began seeing a psychiatrist “who taught me a lot of tools to be able to cope with those negative thoughts and emotions.”
She began paying more attention to her own health and well-being and became more aware of stress triggers. She pulled through.
The bottom line, said Dr. Matthews, is that “doctors are people, too. When it comes down to the core of each of us, we’re all just a person. And sometimes life can overwhelm each of us, no matter how smart you are.
“When you’re drifting in a storm, you really need someone to throw you that lifeline.”
 UT System addresses well-being of physicians
UT System addresses well-being of physicians
The public health care crisis created by physician burnout and depression is being addressed by The University of Texas System, of which UT Health San Antonio is a component.
“As the employer of thousands of physicians, University of Texas institutions have a great stake in assuring that they can thrive despite the many stresses and pressures of their work environment,” said Ray Greenberg, M.D., Ph.D., the UT System’s executive vice chancellor of health affairs. “The UT System aspires to be a leader in developing and implementing strategies to support the well-being of our caregivers."
In September, the UT System sponsored a symposium at The University of Texas MD Anderson Cancer Center in Houston that brought national leaders to discuss the causes, consequences and solutions for physician burnout in academic health settings. A multi-pronged plan includes conducting a systemwide assessment of the problem, creating focus groups and recommending solutions at the clinical, departmental, institutional and system level.
Chancellor William H. McRaven said reducing physician burnout needs to be a priority because of its broad repercussions.
“I think this is a major, major issue … and we have to aggressively address it,” McRaven told the UT System Regents recently. “We can be a national leader in this and we should.”
A journey home
The kid who lived in the “Alamo” house, who spent time in “the projects,” who was 7 when his father died. The kid who was dirt poor, a migrant worker at age 9. Unlikely, maybe, but that kid from Alamo, Texas, grew up and got an education. He’s a doctor now. Yes, Dr. Torres.
But he’ll always be Joel. Joel, whose heart belongs to the Valley.
***

Instinctively, perhaps, Joel Torres, M.D., has always known that highways in Texas’ Rio Grande Valley run both ways. Out, yes. But always back again. The roads took Joel and his family to the asparagus fields of Michigan as migrant workers, and back. They took Joel to places he could receive the finest education imaginable, first to the East Coast, then the West Coast, then to medical school at UT Health San Antonio. And he could have stayed away.
But then he wouldn’t be Joel.
Driving slowly down E. Acacia Avenue in Alamo in his beat-up 2005 Honda Civic, he points out this and that, scenes from his youth. He’s soft-spoken, calm, practical—humble.
He stops in front of one of his childhood homes, now an abandoned cinderblock house adorned with graffiti. The house has a strong resemblance to the Alamo shrine in San Antonio, with its familiar bell-shaped façade.
“I was known as the kid who lived in the Alamo house,” Joel said, chuckling. He recalled a friend down the street, playing in the rubble on the vacant lot next door, being shot by an air gun and his mom having to dig the pellet out. He remembers walking the short block to Ben Franklin Elementary, where he made his second-grade teacher cry by talking about his father’s death.
When his father died in 1986 at age 34, he left 7-year-old Joel, wife Teresa and three other children alone and poor.
Joel’s older sister, Leonor, remembers the difficult days. “Our mom was young, in her 30s, and she found herself alone with four children,” Leonor said. “The struggles were financial, yes, but also emotional. She had to face things head on.”
Teresa, like her husband, was born and raised in Mexico. She spoke only Spanish, had little education and few marketable skills. Without a steady income but with mouths to feed, Teresa made the difficult decision to travel north with her kids to work the fields as migrant laborers. Every summer for eight years, the entire family would pack up and drive to Michigan or Idaho to work from sunrise to dusk. In Michigan they picked asparagus. In Idaho, potatoes and beets.
 They lived in a tiny 10-foot trailer, with the kids in bunkbeds and mom sleeping on the floor. They’d rise between 3 and 4 a.m., every morning. It was grueling, monotonous, back-breaking work.
They lived in a tiny 10-foot trailer, with the kids in bunkbeds and mom sleeping on the floor. They’d rise between 3 and 4 a.m., every morning. It was grueling, monotonous, back-breaking work.
Occasionally, Joel has flashbacks. “I remember sitting on the machines picking asparagus, and you’re kind of hunched over all day. And the machine rolls forward and you’re grabbing the asparagus. It’s cold and your hands are hurting and you have to keep on doing it.”
The field work, supplemented by small jobs such as housecleaning that Teresa would pick up during the school year, sustained the family, but barely. “I realized early on that I was poor,” Joel said. “I learned not to ask for things. Even food became an issue. I started to notice that my mom wasn’t eating until we all did. So I wouldn’t eat until she did, and we’d kind of argue over that.”
When the rent went up on the Alamo house a few years after his father died, the family had to move just blocks away to “the projects,” as he calls them, federal assistance housing where they stayed for a couple of years.
Joel and his siblings readily credit Teresa with the strength of an army in keeping the family together no matter what. Family was the most important theme of her life. Unity. Caring for each other.
And whether in Alamo or the fields, there was one other constant message from Teresa to her kids. “Always, we’d hear, get an education or you’ll be doing [migrant work] the rest of your lives,” Leonor recalled. “Education was everything to her.”
When Joel came home with 95s on his report card, she’d get upset. She wanted 100s.
“[Our mom] absolutely pushed all of us,” Joel said. “She would demand excellence.”
By eighth grade, inspired by an algebra teacher, Joel became a self-described math nerd, joining the math club. “Math was an escape,” he said. “I understood it so well and enjoyed it so much. In summers, I’d read math textbooks for fun. It helped me focus in high school.”
Joel’s intellect was on full display. He graduated as valedictorian of Pharr-San Juan-Alamo High School. And then, a new road beckoned. Encouraged by a teacher, he applied for and was admitted to the Massachusetts Institute of Technology, even though he’d never heard of the prestigious, Boston-area university. Scared to death, he remembers, off he went, a poor kid from the Valley.
At MIT, where he’d eventually earn a mechanical engineering degree, one of Joel’s projects was designing a crib for babies, complete with sensors and alarms that might prevent sudden infant death syndrome, or crib death. It was his first real exposure to the medical field.
Now with an interest in medical devices, Joel entered graduate school at Stanford University to study biomechanical engineering. There he worked on a team designing enhanced intubation devices and vascular access grafts for patients on hemodialysis. And for the first time, he started interacting with patients and physicians. He had found his calling.
“I started thinking, medicine interests me more,” he said. “That world interested me more than the engineering world.”
Determined now to be a doctor, the trained engineer returned to the Valley and what was then UT Pan American to take courses required for medical school. Joel chose UT Health San Antonio partly due to its diversity and, especially, its proximity to his beloved Valley. He became one of a handful of students, many of whom were the first in their families to attend college, much less medical school, offered a full-ride scholarship through the philanthropy of Joe and Teresa Lozano Long.
Joel remembers walking the stage in May 2009 to receive his medical degree. Unlike MIT and Stanford, so far from Texas, his mom and siblings and friends from the Valley were there cheering him on. “It was almost like I was watching myself on TV,” he said. “It was like, is this actually happening? The moment I got the degree it was just a sense of accomplishment, of joy, of knowing that everything that had happened in my life had led up to this moment. I knew my life’s direction.”
Joel spent three years in residency in emergency medicine at the Texas Tech University Health Sciences Center in El Paso before taking the road that always leads home to Alamo and the Valley.
Now 38, married to his wife, Alex, and with three young children, Joel works at a free-standing emergency medicine clinic in Edinburg for Rio Grande Regional Hospital. The family lives in a modest home in San Juan (“only because we couldn’t find a house in Alamo,” Joel said), within a mile or two of his mom, his boyhood haunts, the church he’s been attending since he was a boy, the schools of his youth, the roots of his dreams.
 Aside from the Valley being home, Joel admits that the region’s health disparities also drew him back. Access to care and cultural factors have always been problematic, he said. Hispanics experience higher rates of obesity, diabetes and other diseases, lower rates of health insurance, and less access to health care providers.
Aside from the Valley being home, Joel admits that the region’s health disparities also drew him back. Access to care and cultural factors have always been problematic, he said. Hispanics experience higher rates of obesity, diabetes and other diseases, lower rates of health insurance, and less access to health care providers.
“I have no memories of my dad being well,” Joel said. “I don’t know if it was because my mom and dad didn’t really understand the medical system. But I never remember him going to a doctor for a check-up. The only time he saw a doctor was when he had to go to the hospital. He’d just have to wait until he was very sick.”
His dad, also named Joel, had an infection in his arm so long that it spread into his chest and proved fatal.
“I never remember going to a doctor myself unless something happened,” Joel added. “I guess one of the reasons I chose emergency medicine is because of the way I saw medicine growing up. … It was more of an acute event. If you had a laceration or a broken arm, you’d go to the doctor. But you wouldn’t go to the doctor for a check-up. That didn’t make any sense.”
Joel enjoys the immediacy of ER work. “The most rewarding part is being able to help people right when they need help,” he said.
Most of all, Joel is content being home.
“I love the people down here. I love the area. I know a lot of people don’t,” he said, laughing. “For me it was really about family. And the people are friendly and giving, so it just felt right for me to come home and be of some help to my community. Growing up, we may have struggled, but really it was the helping hands of the people at our church and others in the community who got us through.”
He understands the culture, the people, the way they live their lives and the reasons they do what they do, he said.
“And so for me, now being trained as a physician, I felt like now I have the skills that could help the community,” he said. “I really can’t imagine being a physician [anywhere else].”
 But, in typical fashion, Joel isn’t satisfied with doing good when he can do better. He volunteers at his church, Primera Iglesia Bautista in Alamo, and participated in a medical/mission trip last summer to Senegal in West Africa. He also works at McAllen’s Sacred Heart Catholic Church at a respite center for immigrants.
But, in typical fashion, Joel isn’t satisfied with doing good when he can do better. He volunteers at his church, Primera Iglesia Bautista in Alamo, and participated in a medical/mission trip last summer to Senegal in West Africa. He also works at McAllen’s Sacred Heart Catholic Church at a respite center for immigrants.
His guiding principle, Joel said, has always been to contribute to the community that nurtured him. Watching his kids grow up in the Valley, sending them to a public school, working on common goals to move the Valley forward, are “more important to me than living in a big house in a big city,” he said. “I enjoy being seen as Joel and not Dr. Torres, if that makes any sense.”
Joel met Adela Valdez, M.D., in his last two years of medical school while doing clinical work at the Regional Academic Health Center in Harlingen (now part of the UT Rio Grande Valley School of Medicine). He considers her a role model, and she returns the admiration.
“If you look at his background, he came from very humble beginnings,” said Dr. Valdez, now associate dean of student affairs at the UT Rio Grande Valley School of Medicine. “He went through all these obstacles and on to the best schools in the nation. He just saw obstacles as challenges. He’s filled with humility and compassion and altruism. To me, he’s a servant leader, an incredible human being who happens to be a doctor.”
For Joel, happy that the road has returned him safely home, the goal is to be seen as a good father and a good husband, a good family man. And as a caring physician who’s engaged in the lives of those around him.
“Honestly, I can’t believe it sometimes,’” Joel said. “The places that I’ve gone. Up to Boston. Out to San Francisco. For a lot of people it’s almost like a dream. It’s something that’s difficult to obtain, if not impossible. That’s why I always go back to, it wasn’t my doing; it was the community and the people around me. My mom and brother and sister, they had to work. I owe it all to them.”

Empowering generations

Joel Torres, M.D., was a first-year medical student when the news came: He had been selected as a Long Presidential Scholar in the Long School of Medicine.
It was life changing for the man who had grown up spending summers in the fields as a migrant laborer to help keep food on the table. He was the first in his family to attend college, and by the time he received the Long scholarship, he had already earned a bachelor’s degree from Massachusetts Institute of Technology and a master’s degree from Stanford University.
As a Long Presidential Scholar, he was awarded a full scholarship from Austin philanthropists Joe R. and Teresa Lozano Long. The gift allowed him to focus on getting through medical school without the additional worry of the expense of his education, he said.
“I feel that saying ‘thank you’ isn’t enough to show appreciation to people as generous as the Longs,” said Dr. Torres, now an emergency medicine doctor in Edinburg, Texas. “They have given me a wonderful gift, not only financially, but also the gift of their trust that I honor today by being the best physician I can be.”
The Longs began supporting UT Health San Antonio in 1999, with annual scholarship gifts for 12 medical students from South Texas. Their scholarship provided full funding for each student to complete medical school, and resulted in more than $1 million invested in scholarship support in the early years of the program.
Then came a transformative $25 million gift in 2008. It created the Joe R. and Teresa Lozano Long Scholarship Research and Teaching Fund endowment, which is held in the Office of the President. Each year, the endowment distributes scholarship funding that supports more than 50 students in medicine, nursing, physician assistant studies, and the M.D./Ph.D. program. It also gives annual support for medical research, and funds to establish new faculty chairs that help the university recruit and retain faculty.
That same year, the UT System Board of Regents honored the Longs by naming the university’s Joe R. & Teresa Lozano Long Campus.
Less than a decade later, the Longs stepped forward with an additional $25 million gift to UT Health San Antonio and the Long School of Medicine. When considered in its totality, the impact of the Longs’ giving to the university exceeds $61 million, and that impact will continue to grow, officials said.
On Feb. 14, the Board of Regents officially approved the naming of the Long School of Medicine as the Joe R. & Teresa Lozano Long School of Medicine.
“Their gifts are remarkable for many reasons, but especially for the extraordinary impact they have already had on improving health care access and delivery in South Texas,” said UT System Chancellor William McRaven.
The latest gift established a $1 million distinguished chair endowment for the dean of the Long School of Medicine; a $4 million endowment to provide additional scholarships for students from throughout Texas who are studying to be physicians; and a $20 million President’s Endowment for Faculty Excellence in Medicine held in the Office of the President to support faculty recruitment for the Long School of Medicine.
The Longs met as teachers in Alice, Texas. They most enjoy interacting with young people and supporting their dreams of education. Teresa Lozano Long, Ed.D., and Joe R. Long, J.D., both earned their doctoral degrees from The University of Texas at Austin.
“Good health is a necessity in life,” Joe Long said. “Our goal is to empower generations of young people to enter health care and enhance the quality of life of our state.”
Dr. Torres said he wants to follow the example that the Longs set.
“They came from small towns, got an education, became successful and worked,” he said. “But they used all that to better the community. I want to be seen as a physician who cares for people and for the community as a whole.”
To date, the Longs have supported more than 290 scholarships to more than 115 students.
“The Longs’ gifts touch every new baby delivered, every sick child or elderly patient treated, every lifesaving surgery performed—every aspect of the daily medical practices of each of these young physicians—and their giving will do that and more for generations to come,” said UT Health San Antonio President William L. Henrich, M.D., MACP.
While the students are often profuse in their praise for the couple, the Longs never miss an opportunity to applaud the students.
Like Dr. Torres, many scholarship recipients are the first in their families to attend college, much less medical school, said Teresa Long.
“They prove that if you give them an opportunity, they will work,” she said. “They don’t come here to have fun.”
Joe Long added, “What we consider the real legacy are the students who will be educated as a result of these endowments. They will make a difference in the future of health care for generations to come.”
 “The Long Scholarship has enabled a new generation of physician-scientists to continue the work of translating these basic science discoveries into treatments. With the molecular era in medicine opening the door for targeted treatments for many diseases, physician-scientists have never been more important to the advancement of health care.”
“The Long Scholarship has enabled a new generation of physician-scientists to continue the work of translating these basic science discoveries into treatments. With the molecular era in medicine opening the door for targeted treatments for many diseases, physician-scientists have never been more important to the advancement of health care.”
—Jeffrey Cooney, M.D./Ph.D. candidate
 “The Longs are a substantial part of why I was able to advance my career in a way I never thought possible. I was a mother of two young children when I began my RN program, and their grant enabled me to focus on my family and my studies instead of stressing about extra income. Thanks to their generosity, I advanced to graduate school, and now I have the job of my dreams as a nurse practitioner in a rural community. They believed in me by their investment, and I get to give that gift back every day by working to provide excellent care to my patients. I’m eternally grateful.”
“The Longs are a substantial part of why I was able to advance my career in a way I never thought possible. I was a mother of two young children when I began my RN program, and their grant enabled me to focus on my family and my studies instead of stressing about extra income. Thanks to their generosity, I advanced to graduate school, and now I have the job of my dreams as a nurse practitioner in a rural community. They believed in me by their investment, and I get to give that gift back every day by working to provide excellent care to my patients. I’m eternally grateful.”
—Kirstin Furl, M.S.N., FNP, a nurse practitioner in Floresville, Texas
 “Teresa and Joe’s impact through their contributions to students of UT Health San Antonio will resonate throughout the generations. I can proudly say that this power couple has positively shaped my life and career and, by extension, the lives of my patients and my future children.”
“Teresa and Joe’s impact through their contributions to students of UT Health San Antonio will resonate throughout the generations. I can proudly say that this power couple has positively shaped my life and career and, by extension, the lives of my patients and my future children.”
—Eithan Kotkowski, M.D./Ph.D. GS2 student
 “The Longs’ generous scholarship supported me at a time when I needed it the most. It has allowed me the freedom to choose my path after graduation without the pressures of large student loans. I am grateful for their support and wish them well.”
“The Longs’ generous scholarship supported me at a time when I needed it the most. It has allowed me the freedom to choose my path after graduation without the pressures of large student loans. I am grateful for their support and wish them well.”
—Benjamin William Rhames, 2014 graduate of the physician assistant program, now a PA in the UT Health San Antonio Department of Emergency Medicine
The dead teach the living

"Charlise Suzanne Felts passed away on Friday, Feb. 27, 2015, in Austin, Texas, surrounded by family. She was 67 years old. Suzanne was born on Nov. 18, 1947, in Mount Holly, New Jersey, to Frederick Charles Starn and Charlotte Louise Gregg. She was raised in Chestnut Hill, Pennsylvania, and received a degree in fine arts from Finch College in New York. ...
"Suzanne was passionate about nutritional healing, animals and the arts. She was an equestrian, loved travel, and found fulfillment and joy in caring for others. …”
And then she gave her lifeless body to science, to medical students who would learn from her bones and flesh and muscle and sinew to heal the living. She became their silent teacher.
***
In the winter of 2014, Linda Baker-Webber, coordinator of the Body Donation Program at UT Health San Antonio, received a call from Suzanne Felts. She was dying, Felts explained, and wanted to know more about the program.
“She told me she was interested in it, was considering it, that she had cancer and this was where she wanted to be, but she wanted to meet the people who would be taking care of her,” Baker-Webber said. “That’s highly unusual, to meet a donor, but it was very important to her. So I relayed that to my director.”
After four years as director of the program, Omid Rahimi, Ph.D., had never met a potential body donor, and he didn’t want to start now.
“Our program is anonymous,” said Dr. Rahimi, associate professor of cellular and structural biology who also directs the Human Anatomy Program. “There’s a balance we have to find. We have to separate the fact that this was a person from the fact that this [cadaver in the lab] was a tool, a machine. Otherwise it’s not easy to do what we do. The student has to be able to say, I have a job to do, I have to learn. For me, if I know the person, it would be more difficult.”
But Felts was insistent and continued to call.
“I told [Dr. Rahimi], if you speak with her, you’ll want to meet her,” Baker-Webber recalled.
On her own terms
By all accounts, Suzanne Felts was one of a kind, a child of the universe. She was highly opinionated and stubborn, especially when it came to her health. She was intensely spiritual, if not overtly religious. She was a social being and loved meeting people. All the wonders of nature fascinated her. She reveled in the beauty of art, as both a collector and a
pastel artist.
And deadly cancer ran in her family.
Suzanne grew up in somewhat privileged circumstances in New Jersey and Pennsylvania. Her parents were well off, and she was proud to trace her ancestors back to the Mayflower. When she was 19, she married and moved to a farm in the Blue Ridge Mountains of Virginia, where she had four children before the marriage ended in divorce.
Then it was on to Las Vegas, where she lived for decades and where her interest in nutrition blossomed. She opened a health food business and was keen to learn all she could about natural healing. She eventually met and married a Texan, moving first to Arkansas, then Marble Falls, Fredericksburg and finally Austin.
Two of her sons, twins Massie Wallace and Teddy Wallace, remember her as a free spirit, naturally inquisitive, a jokester who loved April Fool’s Day, an animal lover.
Massie’s wife, Anna, recalls Suzanne feeding all the stray dogs and cats in her neighborhood.
“In fact, there was a family of possums that were welcome on her back porch. She’d feed them every night, even though they’d fight with her own cats.”
But one interest overshadowed all others.
“Nutrition was basically her life,” Massie said. “In terms of taking care of herself, she always wanted to go the most natural route. She had a strong spiritual connection to a higher power. She was very much a person of mind over matter. Meditation, positive thinking, salt lamps, calm relaxing music. Her environment was most important.”
But by 2014, she had already faced seven bouts with breast cancer dating back 34 years. After finding a lump under her arm and learning that cancer had spread throughout her lymphatic system, Suzanne knew the end was near.
She always met the disease head on and on her own terms.
She was absolutely opposed to chemotherapy and never had the treatment, her sons said. She took a variety of vitamins, minerals and exotic supplements. She kept notes over the years of what foods to eat, what not to eat, what exercises to perform. She kept a daily “Life Plan” that outlined a health routine, with entries such as “Put chamae rose under my tongue” and “Eat 2 tablespoons sprouted raw red wheat.”
She didn’t believe in going to traditional doctors unless she absolutely had to, and even then “she’d just put them in their place” if she felt they were wrong, Teddy said. “She’d just debate them, question everything they did.”
And she remained whimsical about life, Massie said.
“Even when she was going to die, she could laugh at her cancer,” he said. “She wouldn’t let it control her. She didn’t pretend it wasn’t there, but she could laugh about it. At one point they put some sort of dye in her to see where the cancer was, and she said, ‘I just lit up like a Christmas tree. It was everywhere!’”
She began thinking of donating her body to science.
“She didn’t want to pass away, but she had accepted it,” said her daughter-in-law, Anna. “It was hard for her to accept that she wouldn’t be around to help people. She saw this as a way for her to express herself and help people learn from her when she’s gone.”
And to Suzanne’s way of thinking, Anna continued, meeting the people she was going to give her body to was an absolute requirement.
“She didn’t give them an option,” Anna said. “She wasn’t going to gift them with her body unless they met her. She said she wanted to see where she was going after.”
The ultimate gift

human body with teaching assistants and fourth-year medical students Dawn Zhao and Matthew McMahon.
Dr. Rahimi is profoundly grateful to body donors and their families.
“The primary benefit of doing dissections on a cadaver is to learn the intricacies of the human body and the beauty of how the body works, how the body functions so well most of the time for so many years,” he said. “It’s the science behind what the physicians will use to treat his or her patients.”
The university accepts around 200 bodies per year. Donors must be 18 and there are no costs involved. (It’s illegal to pay for body donations or parts.) There are only a few exclusions. Donors can’t be obese or emaciated, and they cannot have any communicable diseases or cancer that has metastasized in the abdomen to multiple organs.
The cadavers are used in anatomy classes by first-year medical students, dental students who focus on head and neck dissections, physical therapy students, occupational therapy students, physician assistant students, graduate and biomedical engineering students.
Anatomy workshops for EMT and AirLIFE workers also utilize cadavers, as do physicians learning new surgical techniques or procedures and residents who can practice procedures before treating patients.
Yet the cadavers represent so much more, Dr. Rahimi said.
“This is [the students’] first experience of being exposed to a person who has passed away and recognizing the value of the gift they have received, recognizing the altruistic nature of the person donating themselves for the greater good of humankind,” he said. “I think that really puts in context the career they’re about to embark upon.
“The value of giving and the spirit of love and caring for other people is what they’re gaining. There’s no other way to teach that empathy, that recognition of the importance of patient care, of respect and dignity. The cadaver is their first patient. The student will know more about this person than any other patient they will ever have because they’re going to fully learn the intricacies of this body they’re dissecting.”
Body of knowledge
Despite his reluctance, Dr. Rahimi, along with Linda Baker-Webber, met Suzanne on Dec. 29, 2014.
“She was bubbly. She was a beautiful woman,” Baker-Webber recalled. “To look at her, she was the picture of health. She was warm and very receptive, laughing, smiling, in very good spirits. She was a very joyful woman to meet, but she knew her fate.”
Dr. Rahimi said the meeting turned out to be “one of the most enlightening experiences for me.”
Suzanne was “prolific in telling others about her interest in health and nutrition,” he added. “She wanted to tell that to as many people as possible. And the information she had gained about her body through her research, her experiences with health and her disease, she wanted to give her body as a body of knowledge to us to learn from.
“She was 100 percent interested in, ‘How else can I help? Even in my death I want to be able to help. Here’s my body. Are you going to be able to use it?’”
Anna recalled the day of the meeting.
“I remember her getting ready for that interview,” she said. “She spent hours getting ready to go meet these people. It was really important to meet them and look alive. She said she didn’t want to look sick or for them to remember her as looking sick. She left the house in heels and all made up.
“She didn’t want to just be a body. I know it’s the Body Donation Program. But she said she wanted to give her life to them. I think she accomplished that.”
Suzanne left the meeting comfortable with the surroundings and with her decision to donate her body. Sixty days later, on Feb. 27, 2015, she was dead.
Gone, but not forgotten
Toward the end of each academic year, the Body Donation Program holds a solemn interment ceremony to bury the remains of donors. Faculty, staff, students and the families of the donors gather as bagpipes sound the familiar notes of Amazing Grace, an AirLIFE helicopter performs a flyover and buglers play Taps. Always, students representing each of the anatomy classes talk about the life lessons learned through those who gave themselves as the ultimate gift.
Last April, occupational therapy student Kathryn Crane addressed the gathering.
“There will not be a moment that goes by in our careers that we won’t think about what a blessing it was to have this hands-on experience,” she told the families. “Your loved ones have helped shape us as clinicians, but ultimately because of their generosity, they have helped those that we will treat. The gift they provided us is one that will continue to give and will never be forgotten.”
Supporting a new generation of scientists
Vaccines work because they teach the body to remember—and attack—a particular disease. So Elizabeth Leadbetter, Ph.D., is studying how to enhance the immune system’s memory to identify and attack a disease such as cancer.
Lipid-containing nanoparticles activate B cells and natural killer T (NKT) cells to work together to amplify the body’s memory of the invading disease. If she can harness this process, the body’s memory of the invading disease could be enhanced, which could lead to the detection of precancerous changes in the body and prevent the spreading of the disease, Dr. Leadbetter believes.
“This funding will allow me to apply an approach I had been using to develop a vaccine for an infectious pathogen and apply the same idea to developing an anti-cancer treatment,” said Dr. Leadbetter, associate professor of microbiology and immunology. “If this is as successful as I hope, it should lead to a completely new direction for my lab and will eventually help to make us competitive for other funding opportunities in the cancer arena. I am eager to see if our approach can make a lasting impact in the area of cancer immunotherapy.”
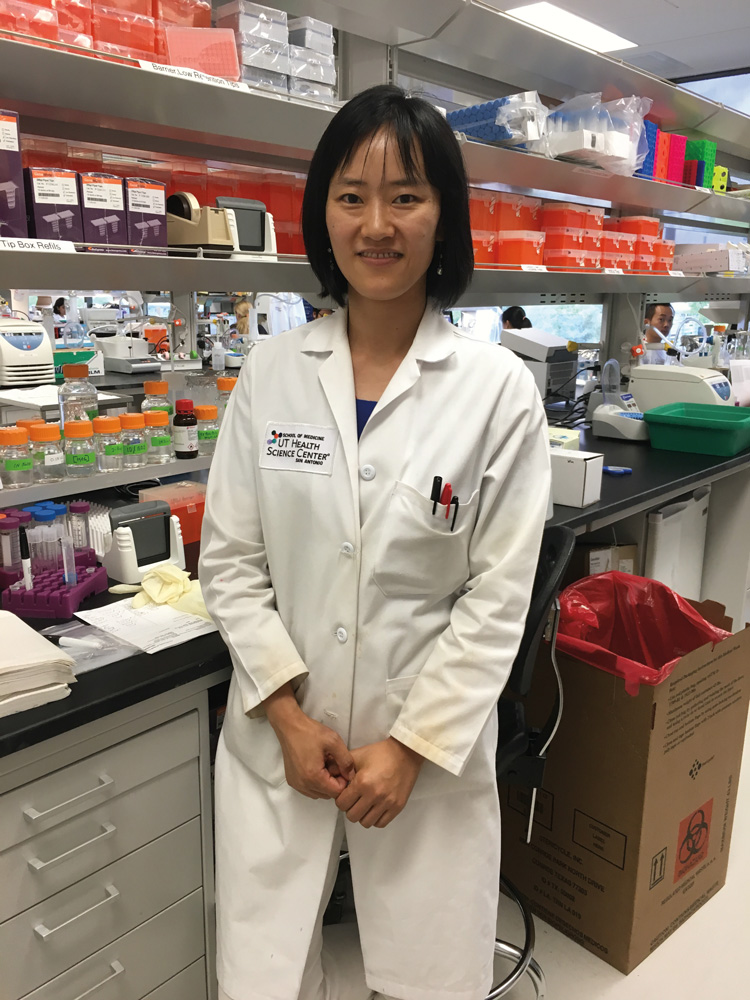
Dr. Leadbetter was one of three junior faculty members in the School of Medicine selected to receive $450,000 over the next three years from the Max and Minnie Tomerlin Voelcker Fund. The money will be used to develop innovative lines of research to make preliminary discoveries that may result in attracting National Institutes of Health-funded research to the city. Xiao-Dong Li, M.D., Ph.D., assistant professor of microbiology, and Kexin Xu, Ph.D., assistant professor of molecular medicine, were also recipients of $450,000 to advance their work.
“Voelcker Fund awards help junior scientists to establish a track record of success,” said William L. Henrich, M.D., MACP, university president. “The focus of our awards in 2016 is cancer, a disease that is, in its complexity, a thousand diseases.”
Dr. Li’s research focuses on the DNA of tumors. He has discovered a molecular pathway the immune system uses to recognize and attack abnormal DNA. A vaccine to boost this pathway could be very effective in fighting cancerous tumors, in addition to fending off viral threats, he said.
Dr. Xu seeks to understand the link between cancer and metabolic disease such as obesity and diabetes. She focuses on epigenetics, the study of biological processes that switch genes on and off without altering the genetic code itself. Epigenetic changes may be prompted by the environment, diet, stress, aging and other factors.
“The Voelcker Fund is impressed with the quality of the investigators and their research,” said Banks M. Smith, a Voelcker trustee. “We know strides will be made to help find cures for cancer.”
Since 2007, the Voelcker Fund has given more than $18 million to the university. In addition to the Young Investigator Awards, the fund also supports other university initiatives, such as the Voelcker Biomedical Research Academy, which provides an immersive biomedical research education and college preparatory program for San Antonio-area high school students.
Dr. Leadbetter pointed out that in a time of declining government support for scientific research, funding by philanthropies such as the Voelcker Fund is vital.
“Without it,” she said, “we could lose an entire generation of scientists.”



 De Medicina, by Aulus Aurelius Cornelius Celsus (c. 25 B.C.–c. 50 A.D.)
De Medicina, by Aulus Aurelius Cornelius Celsus (c. 25 B.C.–c. 50 A.D.)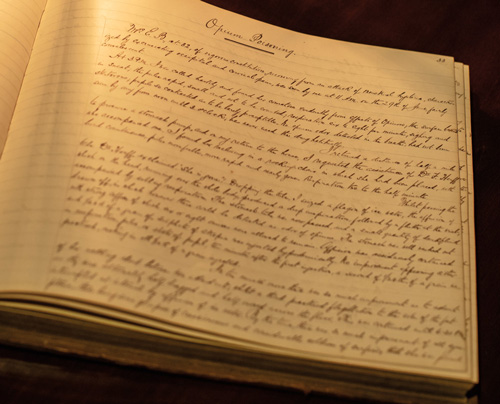 Cupples Casebooks, by Dr. George Cupples (1815–1895)
Cupples Casebooks, by Dr. George Cupples (1815–1895) De humani corporis fabrica libri septem (The Fabrica), by Andreas Vesalius (1514–1564)
De humani corporis fabrica libri septem (The Fabrica), by Andreas Vesalius (1514–1564)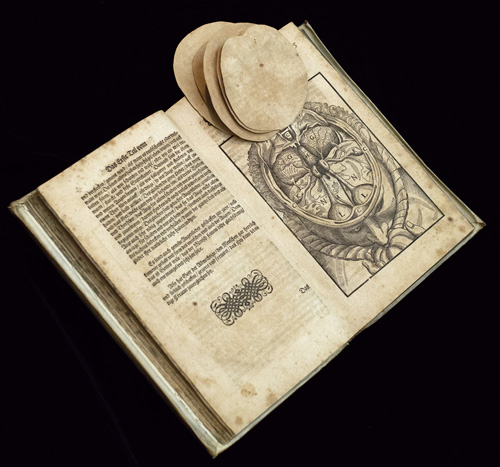 Ophthalmodouleia, by Georg Bartisch (1535–1606)
Ophthalmodouleia, by Georg Bartisch (1535–1606) Canonis libri V, by Abu ‘Ali al-Husayn ibn Sina (known in the West as Avicenna) (980–1037)
Canonis libri V, by Abu ‘Ali al-Husayn ibn Sina (known in the West as Avicenna) (980–1037)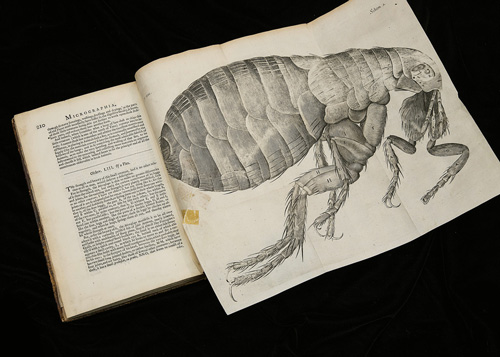 Micrographia, by Robert Hooke (1635–1703)
Micrographia, by Robert Hooke (1635–1703) Medical bag and instruments belonging to Dr. John Matthews (1908–1995)
Medical bag and instruments belonging to Dr. John Matthews (1908–1995)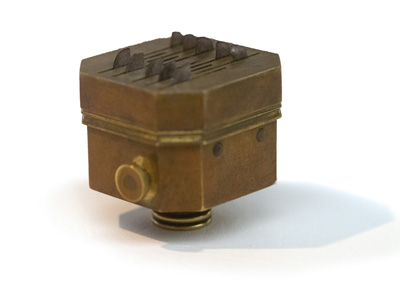 Bloodletting instruments
Bloodletting instruments



