Behold, the Magentist!
A legacy of illusions eases patient anxiety and inspires the next generation through magic and dentistry
There’s something enchanting about the world of dentistry when you add a little bit of magic into the mix.
For Benjamin Taylor, DDS, a retired pediatric dentist who returned to volunteer as a UT Health San Antonio School of Dentistry adjunct professor, magic was the perfect antidote to patient anxiety.
Early in his career, Taylor began incorporating sleight of hand into his pediatric practice, and it wasn’t long before it became his signature method for easing the dental anxiety that’s common among young patients.
For Francisco “Javy” Garza, a third-year student at the School of Dentistry, Taylor’s tricks helped him get through childhood dental visits and inspired him to carry the wand and use it in preparation for his own practice. While Garza was first inspired by Taylor’s tricks as a child, it wasn’t long before he was learning magic himself. By middle school, Garza was performing illusions at birthday parties and family events.
“It’s a fun way to bond with people,” Garza explained.
A touch of magic
Taylor’s love for both dentistry and magic started long before his tenure as faculty for UT Dentistry’s Greehey Family Foundation Pediatric Dental Clinic. His career path, an unlikely but fitting blend of both, began in a U.S. Air Force training program.

“I had the chance to work as a dental assistant, and that sparked my interest in the field,” Taylor said.
But it wasn’t until years later, after a stint in dental hygiene, that he found his true calling in pediatric dentistry. Taylor soon discovered an unusual way to break the ice with his young patients — magic tricks.
Inspired by a fellow dentist and 1983 School of Dentistry alumnus, C. Roger Macias Jr., DDS, who used magic as a tool to soothe children in the dental chair, Taylor started incorporating small illusions into his practice.
“I began showing kids simple tricks like making a scarf disappear or making sponge rabbits multiply in their hand. The change in their demeanor was instant,” Taylor recalled.
Soon, magic became his signature method for easing nervous little ones, allowing them to relax and forget about their dental fears.
“I always made it a point to show each child a magic trick at the end of their visit, no matter what. It gave them something to look forward to and left them with a smile.”
‘From fear to wonder’
As a bonafide magician, Taylor’s magic is more about creating an experience that sparks trust with his patients. Perhaps the most profound magic trick that Taylor performed was not pulling rabbits out of hats, but rather, the bond he created with patients like Garza.

Garza now feels that Taylor’s magic was not only an entertaining distraction, but also a turning point in his life. He was just a child when he first saw Taylor perform a trick during a dental visit within the Pediatric Dental Clinic at the Ricardo Salinas Health Center. Recalling that he was a nervous patient, Garza remembered his experience with startling clarity.
“I was terrified of going to the dentist, but when Dr. Taylor pulled out a deck of cards and began his tricks, all of a sudden, I forgot to be scared,” Garza said. “He made me feel like I was part of the show. It was his kindness and patience, combined with the magic, that made me trust him.”
Garza already had strong ties to the dental profession through his parents’ work as dental lab technicians, but this moment was transformative for him.
“After that visit, I knew I wanted to be a dentist. Dr. Taylor’s tricks showed me that dentistry didn’t just have to be about procedures — it could be about connection, too,” he shared.
Now, one year from graduation, Garza has continued the tradition of using magic to build trust with his own patients. Doing a quick sleight of hand with a deck of cards or a coin trick, Garza has found that, much like he once did, his patients begin to relax and open up.
“It’s all about breaking the ice and creating that sense of curiosity. Magic has this power to shift a patient’s mindset from fear to wonder,” Garza said. “And that’s the key to building rapport. When you make a patient comfortable, they’re more likely to trust you, and trust is everything in dentistry.”
More than a gimmick
Taylor was delighted to hear of Garza’s success and the ripple effect his magic has had.
“It’s incredible to see how the things I did as a dentist have inspired Javy,” he said. “He’s taken it to a whole new level, making magic a part of his daily practice. That’s the beauty of mentorship. It’s about passing on a legacy — one that isn’t just about technical skills, but about human connection.”

Both Garza and Taylor agree that magic and humor are powerful tools in health care.
“In dentistry, we’re not just treating teeth; we’re treating people. And if you can make a person feel comfortable and understood, you’re already halfway there,” Taylor said.
In fact, research suggests that incorporating entertainment into health care can reduce patient anxiety. For instance, some studies show that humor and distractions like magic tricks can lower stress, reduce heart rate and create positive memories associated with dental or medical visits. The concept has been around for decades, but it continues to inspire originality in the way health providers approach patient care.
Garza believes that the lessons he learned from Taylor are not just smoke and mirrors; they’re about creating an environment where patients feel heard, valued and cared for.
“As a future dentist, I want to make sure that every patient walks out of my office feeling treated but also truly seen and respected,” Garza said. “And if that means showing them a magic trick to help them feel more at ease, I’ll do it every time.”
Magical mentors
For Taylor, the magic doesn’t stop at the clinic; he is also passionate about sharing the art with his peers. Once he was even invited to speak formally during a seminar at the American Academy of Pediatric Dentistry in 2013, where he introduced fellow professionals to the therapeutic benefits of magic in dentistry.

“I wanted to inspire more dentists to use magic to build trust and reduce fear,” Taylor said.
However, not every patient has been easily charmed through the years. One particularly tough crowd came from children whose father was a professional magician.
“They were a hard sell,” Taylor laughed when remembering the encounter. “But that’s part of the fun!”
Like Taylor, Garza believes in sharing his knowledge with others, teaching his fellow classmates simple sleights of hand to help equip them with ways to relax and bond with their own patients.
“It’s all about breaking the ice and making the patient feel more at ease,” Garza explained.
Further solidifying their commitment to the craft both inside and outside the clinic, Garza and Taylor hold membership with professional magic clubs. Although both “magentists” remain eager to pass on their craft, they still keep some surprises up their sleeves.
“In magic, there’s a certain code,” Garza said. “We don’t reveal all our secrets. Some tricks require practice and skill, and for those, it’s important for people to buy the props and learn the techniques themselves. It’s about respecting the craft and ensuring the magic remains just that — magical.”
Explore your alter ego: What drives personal happiness can fuel professional success
Learn what inspires some of your colleagues to make lives better, both on and off campus
Clark Kent and Superman. Dr. Jekyll and Mr. Hyde. Beyoncé and Sasha Fierce.
Alter egos aren’t only for superheroes and superstars. In a quest to discover the multifaceted personas around UT Health San Antonio, we recently invited our university community to reveal their alter egos. The responses poured in, and we were not disappointed. We were amazed.
Which raises the question: How well do you know the people you chat with in the breakroom or see in the lecture hall? Each of us is more than our particular focus at work or in the classroom or lab, and often what we do in our off-hours energizes the passion we bring to our work and studies.
In this compilation of alter egos, learn what inspires some of your colleagues to make lives better, both on and off campus.
Brian Purcell: Texas Highway Man

By day, Brian Purcell is an IT security systems architect in the Department of Information Technology Security Engineering who navigates the complexities of its ever-changing technology. But outside the office, he’s better known as the “Texas Highway Man,” a local legend when it comes to all things transportation.
With a lifelong passion for roads, highways and urban planning, Purcell has spent decades curating his website, TexasHighwayMan.com, where he shares comprehensive insights into local roadways. His deep knowledge even earned him the prestigious Road Hand Award from the Texas Department of Transportation in 2020 for his contributions to preserving San Antonio’s transportation history.
“Typically, this award is given to local politicians and community leaders who help champion projects or otherwise have supported TxDOT’s efforts in their communities, so as someone who is neither in the road construction business nor politics, it was quite a surprise and honor to receive this recognition,” Purcell said.
His interest in transportation was enriched by time spent in Germany, where he gained an appreciation for trains and public transit, a subject he continues to explore through his companion website.
With a busy family life and a full-time career, Brian’s alter ego shines as a quiet community resource, helping San Antonians navigate their roads with precision and passion. His knack for directions and his ability to simplify complex transportation issues have made him an unsung hero of the roadways.
Kelley M. K. Hitchman, PhD, MS, F(ACHI): Top organ donor
At work, Kelley M. K. Hitchman, PhD, MS, F(ACHI), pairs kidney donors with recipients, helping to save lives one transplant at a time. But her commitment to the cause goes beyond her professional life.

In 2021, Hitchman made the remarkable decision to donate one of her own kidneys to a stranger, a life-changing experience that ignited a new personal mission — scaling the summit of Mount Kilimanjaro as part of an international Kidney Donor Athletes team. Her goal? To raise awareness for the need of kidney donation and to inspire others to become donors.
“Fear holds a lot of people back from donating a kidney, or a portion of their liver,” Hitchman said. “One of the most vocalized myths is that most folks don’t have the same quality of life and health after living donation. What better way to prove that this myth is just a myth than to climb the tallest freestanding mountain in the world — with one healthy kidney.”
She reached the top of the iconic mountain on World Kidney Day, March 14, 2024, in honor of her work and the many lives touched by kidney transplantation.
“Living organ donors can continue to live full and active lives in every way,” she said. “I am fortunate to know many donors who participate in marathons, triathlons, weightlifting, cycling — you name it! Donors continue to live normal lives following donation with no restrictions.”
Hitchman said that most donors are advised to refrain from vigorous activity or heavy lifting for about eight weeks following donation, but after that, “life moves on. I walked around the hospital the day after my donation without assistance,” she said.
“I did not require any pain medication by the third day after my donation, and I could walk four miles within a week of donation. I continue to work full time, exercise and parent my two children without at all physically noticing that I only have a single kidney. The donation was a wonderful experience for me — one that I wish everyone could experience.”
Hitchman is an associate professor in the Department of Pathology and Laboratory Medicine in the Joe R. and Teresa Lozano Long School of Medicine and the Malú and Carlos Alvarez Center for Transplantation, Hepatobiliary Surgery and Innovation. She is also the section chief and director of the Histocompatibility and Immunogenetics (HLA) Laboratory at University Health.
“Normal people can do extraordinary things and can keep living full and active lives,” she said.
Macie Randol, BSN, RN: Heart Healer

Macie Randol, BSN, RN, is the dedicated primary care nurse at the School of Nursing’s Wellness 360 pediatric clinic, located at Respite Care of San Antonio, a foster home for children with developmental disabilities and their
neurotypical siblings. During the workday, she provides primary care services to the children in residence, though her care extends beyond just meeting their physical health needs.
“My heart really grew towards these kids,” Randol said. “I kept thinking, ‘I don’t have any control over where they came from or where they’re going next, but maybe I can teach them to have faith.’”
Every other Sunday, she shifts from devoted nurse to faithful guide by leading a voluntary-attendance children’s church program at the foster home in her free time. On those days, toddlers to teens gather in the group home’s large dining room.
“We watch a video Bible story and then do a craft or activity together, allowing time for the kids to ask questions or just enjoy some time together. Sometimes, I have three kids join, other times I have 15 kids,” she said.
Her leadership has built a sense of community and belonging among the children, creating strong, lasting bonds that go beyond traditional caregiving. Through this experience, the children now see Randol as more than just a nurse. By knowing that time with her isn’t always about a clinic visit, it has helped them feel more comfortable and cared for, both in body and in spirit.
Carlos Hernandez: First-gen overcomer
First-generation graduate and first-year dental student Carlos Hernandez has faced a challenging path to be where he is now, including the experience of his childhood home burning to the ground. Raised alongside his seven siblings by a single mother, first in Mexico and then immigrating to the U.S. as a boy, Hernandez learned early on the value of hard work.

Every summer, he and his brothers worked on fields in Indiana to earn money for school clothes, guided by their mother’s wisdom that anything worth having must be earned. His grandfather pushed him to pursue his education by reminding him that without a focus on his future, he could spend his life in those fields.
Hernandez credits his family and Mexican-American heritage for teaching him resilience, the importance of community and a deep sense of responsibility.
“I grew up in a household where taking the first step was the hardest part,” he said. “As a first-generation Latino student, we often don’t have guidance and are afraid to take risks. My mother always told me, ‘Vergüenza es que te pesquen robando, no por andar pidiendo ayuda,’ which means, ‘Shame is getting caught stealing, not asking for help.’ This reminder has helped me overcome fear and push forward.”
These lessons influence how he approaches life, and now, patient care. For those who, like him, face barriers to accessing health care, Hernandez’s goal as a future dentist is to ensure that all his patients receive the care they deserve, regardless of their background.
Matthew Schott: Volunteer master

Matthew Schott, a radiation safety specialist in the Department of Environmental Health and Safety, has found a way to live out his values through meaningful volunteer work with the San Antonio Food Bank, Habitat for Humanity and other organizations. Currently a master’s student studying philosophy, Schott’s academic focus on ethics and human values has led him to explore practical ways to make a difference, and volunteering has provided him with real-world insight into concepts like duty, responsibility and the greater good.
“So, for me, this was an easy decision,” Schott said after learning that the food bank also services the region of Southwest Texas. “Not only could I help my community, but I could also help smaller communities surrounding San Antonio. The San Antonio Food Bank also works with another nonprofit called DaisyCares that provides for pets. It is incredible what these two organizations can do with the money, food and time that have been donated.”
Schott has sorted food, organized food drives and served meals. Through Habitat for Humanity, he has worked to build affordable housing, witnessing firsthand the appreciation and hard work of families.
“It is an incredible feeling to work side-by-side with the future owner of the house you are working in,” Schott said. “The homeowners and their families are always so grateful for whatever help is there for them.”
He sees this work as an opportunity to live out his principles through community involvement.
“Food and shelter are basic essentials, and they are critically important for our survival and well-being. Ultimately, volunteering requires so little on my end, but it offers so much to those in need,” he said.
Schott’s goal is to inspire others to join him in giving back, knowing that even small actions can have a lasting impact on the lives of those in need.
Samantha Gonzalez-Davis: Foosball maven
Samantha Gonzalez-Davis, office manager for the School of Health Professions, is very clear about her goal as a competitive amateur foosball player: She wants to win a national championship title.
“There’s no stopping me right now,” she said.

Gonzalez-Davis started playing foosball in 1987 when she met the man who would become her first husband.
“A year later, we started traveling together. We won our first title. It was mixed doubles. I was just glued. I wanted to do it more.”
But Gonzalez-Davis stepped away from the sport after her husband died in 1994. “It was just a constant reminder,” she said.
After a 25-year break, Gonzalez-Davis returned to foosball at the urging of a friend. She now plays goalie and has won awards for her skill in that position.
“I went back on Feb. 19, 2019, and I have been playing ever since,” she said, estimating that she has competed in at least 2,000 tournaments — more than three dozen in 2024 alone.
“I travel. I’ve gone to 17 states,” she said. “I’ve played against Canadians, I’ve played against Romanians, I’ve played against Italians. Everybody from everywhere comes. You become family; you become friends.”
Beyond the camaraderie and the opportunity to learn new techniques, Gonzalez-Davis enjoys the thrill of competition and the pursuit of victory. To get there, she p
ractices two to three hours a day at home.
“I want to win,” she said. “I want people to know who I am on the table. I just want to be able to get on the table and say, ‘I’ve done it.’ Period.”
Jorgie Ann Contreras, PhD, MSN, RN, CPN: Cover band star
By day, Jorgie Ann Contreras, PhD, MSN, RN, CPN, is an associate professor/clinical in the School of Nursing. But in her off-hours, Contreras strikes a different chord. She has been singing since she was five years old, performing everywhere from church and school choirs to talent shows.
“Currently, my husband and I are in an acoustic cover band called Wasted Talent. We perform together in and around San Antonio,” she said.

Her love for music extends beyond the stage, shaping her life as a form of self-care and family bonding. For the past decade, Contreras has had the honor of singing the National Anthem at the San Antonio Stock Show and Rodeo Cattle Sales, and this year she performed at a San Antonio Missions baseball game.
“My son plays baseball, and we are huge fans of the sport, so being able to sing at the Missions game was such an honor and so much fun,” she said.
Some of Contreras’ most cherished memories include her children joining her to sing and play instruments on stage or at home.
“My daughter sings and plays the piano, and my son plays the drums and guitar every now and then,” she said. “During COVID, we used to do live shows on social media from our living room to help entertain anyone who was stuck in quarantine. Music truly bonds us as a family.”
Drawing inspiration from a wide range of artists, Contreras enjoys engaging with audiences by taking song requests to create an unforgettable experience, which even fueled her own educational endeavors.
“Music actually inspired my dissertation study for my PhD,” she added. “My dissertation title was ‘The Effects of a Music Intervention on Stress, Anxiety and Academic Performance Among New Undergraduate Nursing Students.’”
Her research found that the students who listened to music experienced a significant drop in their anxiety levels after intervention, which was measured by a test called the State-Trait Anxiety Inventory, or STAI. The drop in anxiety was very unlikely due to chance based on her statistical results (p < .001). The same was true when examining changes in anxiety levels, demonstrating music’s positive impact on reducing both stress and anxiety.
Zachary Borrego: Martial arts mentor
Zachary Borrego, a web content producer in the Department of Marketing, Communications and Media, comes from a family deeply rooted in martial arts. Growing up in his father’s gym on the south side of San Antonio, he developed a love for it at a young age, eventually competing in tournaments worldwide. As a teenager, Borrego was selected to represent the U.S. in an international taekwondo tournament in South Korea.

“That was really the first time I saw how far martial arts could take me,” he said. “The competition is what I’ve always loved.”
Although he shifted focus to football in high school, which led to a spot on the Angelo State team, his passion for martial arts remained. After graduating and returning to San Antonio, Borrego reignited his martial arts journey. In December 2021, he had his first fight.
“I ended up turning pro a year later and have been at it ever since,” he said. His dedication and love for the competition keep him focused, and the discipline required for training has taught him valuable lessons that extend beyond the mat, such as respect, humility and a willingness to look beyond first impressions.
“I think sometimes people just see the fighting aspect of [mixed martial arts]. It does seem very barbaric, and people may think we are some sort of savages,” he said. “Most MMA fighters are the nicest people on the planet and have the utmost respect for every opponent and everyone outside of the cage. It’s just a passion and a desire to be the best you can be.”
Training to be the best is a challenging process, but one that’s paid off for Borrego. He’s competed on ESPN’s Contender Series, an opportunity to try out for the Ultimate Fighting Championship, or UFC, and has headlined fights in San Antonio, where he said the local support has been overwhelming.
Borrego also values giving back, especially to fans from the younger generation who look up to him as a role model at his gym. “It’s a role I’ve slowly embraced and grown into,” he said.
Balancing a fighting career with his work in the digital workspace at UT Health San Antonio has been challenging, but his drive to excel in both areas is clear.
“How you do one thing is how you do everything,” he reflected, a philosophy that guides him both in the gym and at the office.
What’s your alter ego? Share your story or story idea at communications@uthscsa.edu.
Discussing death: Teaching students to tackle a taboo topic
Integrating palliative care competency into nursing curricula prepares students for the complexities of end-of-life care
Few words hold as much weight as the ringing echo of “death” uttered in a room.
Despite the discomfort that can accompany discussions about death and dying, this largely taboo topic lies at the heart of every serious injury, illness and end-of-life journey. Yet imagine a patient’s expectation when facing their most vulnerable moment. They rely on their health care providers to navigate this delicate conversation with grace and expertise.
Enter Megan Lippe, PhD, MSN, RN, ANEF, FPCN, FAAN, a palliative care educator who confronts the silence surrounding mortality head-on. As an associate professor at The University of Texas Health Science Center at San Antonio’s School of Nursing, Lippe champions a bold teaching strategy: Learn to embrace the “D” word.
“How can someone talk to their patient about death if they aren’t even comfortable saying the word?” asked Lippe. “The principles of communication are important for this process. We have to balance the need to prepare patients and their families for the possibilities ahead while also understanding the power of silence and giving them space when they are facing these difficult situations.”

Lippe’s job — and her passion — is to ensure each new graduate leaves their program as a competent member of the health care team. That means they enter professional practice well-versed in addressing not only the physical symptoms of someone enduring a serious illness or injury, but also the psychosocial, emotional and spiritual needs of the patient and their family.
Need to know
In 2021, the American Association of Colleges of Nursing (AACN), an organization that establishes quality standards for nursing education, deemed palliative care an essential competency.
“The association updated their curricular guidelines, and as part of that, hospice, palliative and supportive care was named as one of four critical spheres of undergraduate and graduate nursing education,” Lippe said. “It went from nice to know to need to know.”
The Essentials: Core Competencies for Professional Nursing Education, AACN’s educational framework for baccalaureate and graduate nursing programs, provides specific guidance for the development or revision of a curriculum for each degreed program, including core competences each new graduate must exhibit.
While AACN deemed palliative care a basic human right and beneficial at any stage of a serious condition, Lippe said “nurses cannot practice what they do not know.” The End-of-Life Nursing Education Consortium, in partnership with AACN, updated its document of palliative care competency statements for undergraduate and graduate students. These statements are known by nurse educators and students as Competencies And Recommendations for Educating Nursing Students, or CARES and G-CARES (for graduate education), respectively, and are guidelines essential for enhancing care quality, supporting nurses’ professional growth and ensuring culturally competent care.
“Palliative care did not change with these updates,” noted Lippe. Rather, the language around competency was updated to better align with the new curricular standards to make them more meaningful for schools of nursing.
“We are now really speaking to the role of the nurse when patients are seriously ill or actively dying.”
One such statement now reads: “Provide culturally sensitive care that is responsive to rapidly changing physical, psychological, social and spiritual needs during the dying process and after death.” Students can now be assessed based on how well they adjust to changing needs during the imminent death period.
As one real-world example, Lippe recounts a story she often shares with students about taking care of a patient from Mexico.
“The chart documented his religion as Catholic, but [he was] Jewish. Someone made an assumption instead of asking about his spiritual or religious beliefs,” said Lippe. “These details inform how we care and interact with our patients and their families. We can unintentionally do harm by making assumptions. Every person is unique, and we must be proactive in respecting each of their values, beliefs and preferences.”
Simulating reality
Adding to her belief that nurses cannot practice what they do not know, Lippe said nurses cannot know unless they practice, and that they should practice in a safe and controlled environment.
Simulated experiences are a valuable component of nursing education, and Lippe has created several simulations inspired by real-life scenarios she experienced. One simulation walks students through several interactions with a family of a seriously ill patient that leads to the withdrawal of life-sustaining measures.
“I designed the first part to begin with the family not fully understanding what’s going on with their family member,” Lippe said.
“How long will he need the tracheostomy? We are going to Paris in one month. Will it be out by then?” asks an actor portraying the patient’s wife during the simulation. The students are tasked to interact with the family, providing information and comfort while their instructor observes.
The exercise then requires students to assess the patient and communicate with the physician. Students might use the popular SBAR (situation-background-assessment-recommendation) communication framework to identify the problem and, based on pertinent information about the patient and the patient’s condition, consider options and recommend actions.

The final phase of the simulation is Lippe’s favorite.
“After the family meets with the physician, the students further explore treatment options with them. The wife of the patient decides to withdraw life-sustaining measures, specifically the ventilator and medications to sustain blood pressure,” Lippe said.
“I love that part, to see how their jaws drop because they expect the wife to be in denial or fight for her husband’s life, so they’re like, ‘Huh?’ This situation teaches them to be prepared for families to surprise them and to quickly adapt to support their decisions, wherever the patient and family are in their journey with a serious illness,” said Lippe.
A debriefing session follows each part of a simulation to discuss the communication, care and strategies used, as well as how students felt about the experience.
“I like the idea of putting students in a simulation scenario first. It’s a safe space for them to practice and develop their care and communication strategies and receive feedback,” Lippe said.
“When we think about patients who are actively dying, it is a sacred space. We want students to be as prepared as possible to provide holistic, quality care to patients and families when they enter these sacred spaces.”
CARES competency
Achieving competency is at the heart of the knowing and practicing cycles. Nursing educators across the nation are working to enhance their curricula to teach palliative care content and assess competency, said Lippe. To support them in this endeavor, Lippe leads a national team of nursing faculty and palliative care nursing experts who are developing helpful resources through the End-of-Life Nursing Education Consortium.
“CARES and G-CARES are very broad but intended to be really helpful for curricular guidance,” Lippe said. “We also needed a competence assessment regarding specific observable behaviors of students — some way to verify that students can actually do those behaviors by graduation and demonstrate an ability to provide palliative care.”
Putting their collective experiences together, the team produced a primary palliative care nurse competence model and assessment tool, a student assessment tool that connects clinical behaviors to the CARES competency statements. It also works in conjunction with other supporting documents the team created to map each CARES statement to curricular guidelines in AACN’s Essentials framework.
“To go back to our [simulation] example, the role of a nurse is to adjust care to a patient’s rapidly changing needs physically, psychologically, socially and spiritually when a patient is dying,” Lippe said. “Is a student able to adjust through the care process based on a patient’s condition or not? If a student is in a simulation or at the bedside, I can actually watch them do this and evaluate it.”
Rethinking palliative care
For Andrya R. Rivera-Burciaga, DNP, APRN, FNP-BC, ACHPN, a student in the School of Nursing’s PhD in Nursing Science program, having a faculty member on staff who is an expert in this area and who is creating tools on behalf of the profession is beneficial.
“As an advanced practice nurse, I feel there is still a perception in the profession that palliative care isn’t as important as other spheres of care, but the updates to nursing education and tools such as these will bring an awareness that palliative care is valuable,” she said.
Lippe believes it is important for educators to see that their students are already at the bedside of so many patients who would benefit from palliative care.
“As educators, we need to re-envision and expand the who, what, where, when, why and how of palliative care education to ensure we prepare future nurses and health care professionals who will care for these patients and their families,” Lippe said.
“In taking a step back to realize where nurses are taking care of patients with serious illnesses, we find it is everywhere. Palliative care is needed throughout our community because that’s where our patients who have a serious illness live,” said Lippe.
“Our goal is to empower the workforce to improve the quality of life of patients and families living with serious illness across the disease trajectory and at the end of life.”
The future of palliative care
Because of her multifaceted expertise and dedication to advancing nursing education and palliative care, Megan Lippe, PhD, MSN, RN, ANEF, FPCN, FAAN, has been awarded fellowship into three esteemed organizations: the American Academy of Nursing, National League for Nursing’s Academy of Nursing Education and Palliative Care Nursing.
“Dr. Lippe is an exceptional leader, and she is contributing much to the advancement of care for the seriously ill by preparing our nurses,” said Betty Ferrell, PhD, FAAN, FPCN, CHPN, the principal investigator of the End-of-Life Nursing Education Consortium. “Her years of work in creating curricula, innovative teaching strategies and evaluation methods has reached over 1,100 undergraduate and 375 graduate programs.”
ELNEC is a national program dedicated to improving palliative care by equipping nurses with training in skills such as pain management and communication.
As a member and regional chair of the consortium, Lippe is working with other nursing faculty to shape the future of palliative care education. She is the lead author of the End-of-Life Nursing Education Consortium curricula, as well as the American Association of Colleges of Nursing-endorsed national palliative care competence statement revisions for both undergraduate and graduate education.
Lippe’s collaborative research efforts have likewise produced new quantitative measures to assess primary palliative care curricula and competence for advance practice and entry-to-practice nurses.
Four spheres of care
- Wellness, disease prevention. Promotes health and prevents illness through education, lifestyle modification and early-detection strategies
- Chronic disease management. Manages long-term conditions to optimize quality of life and minimize disease progression through ongoing care and support
- Regenerative/restorative care. Restores patient health and functional abilities following acute illness or injury through rehabilitation and recovery-focused interventions
- Hospice/palliative care. Provides compassionate care to relieve symptoms and improve the quality of life for patients with serious, life-limiting illnesses, including end-of-life care
Source: The Essentials: Core Competencies for Professional Nursing Education, American Association of Colleges of Nursing, 2021 (fig. 2, pg. 19).
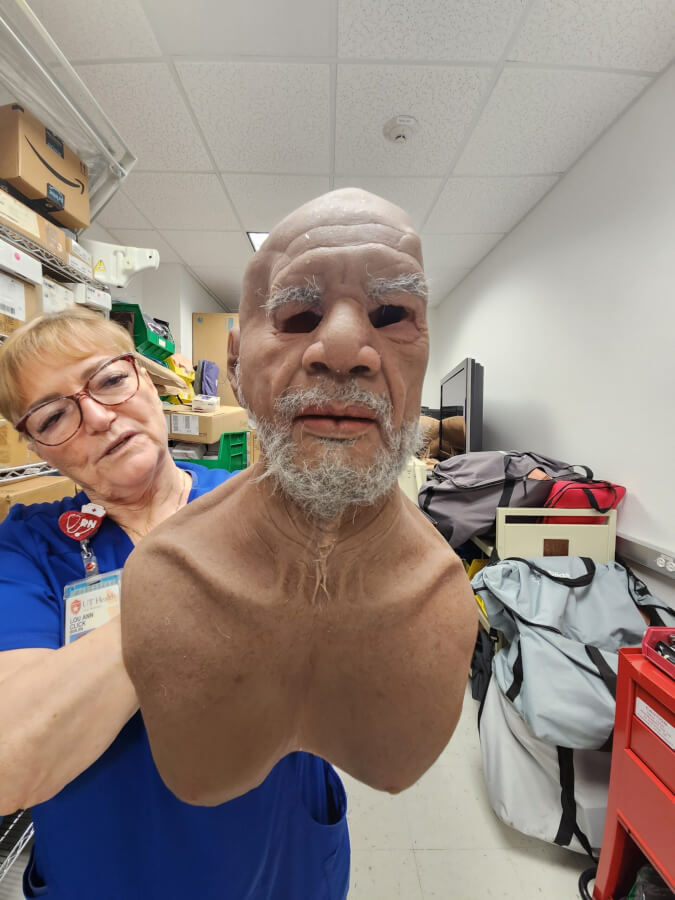
What lurks in the School of Nursing's basement?
It was a dark, quiet evening at the School of Nursing, the kind where shadows stretch long and every sound seems to carry an eerie echo. The halls were nearly deserted.
With the soft hum of fluorescent lights flickering overhead, one lone housekeeper made his nightly rounds, pushing his supply cart through the hallways of the Center for Simulation Innovation when he heard it — a faint, unsettling moan coming from one of the rooms.
Heart pounding, the housekeeper froze. The sound grew louder the closer he crept toward the door. Slowly, he peeked inside.
There, on a gurney, lay a figure. Motionless at first glance, but then… it stirred.
The housekeeper’s breath hitched, a chill running down his spine as the figure let out a soft, low groan.
The dim lighting cast shadows on its face, making it seem all too real. Panic gripped his chest, and before he could think, he let out a blood-curdling scream, abandoning the cart and bolting down the hallway.
Later, campus police would say the gentleman had refused to return to his post that evening.
The culprit behind the haunting? One of the school’s most advanced medical manikins, left powered on after a long day of training students in realistic patient care scenarios.
As spooky season descends, true stories such as this add a playful twist to the essential work happening inside the School of Nursing’s Center for Simulation Innovation, where some of the most sophisticated medical simulators are helping to prepare practice-ready nurses.

LouAnn Click, BSN, RN, simulation lab manager, fondly recalls moments like this — where the realism of the manikins has even fooled nursing staff and, occasionally, students.
“Our simulators are so advanced, they can mimic nearly every aspect of patient care,” said Click, who has been with the school for nearly 25 years. “We have manikins that can track you with their eyes or exhibit real-time changes in heart rate and lung sounds, they offer invaluable training experiences.”
In fact, one manikin, known as Miss Vivian, even had a run-in with U.S. Customs and Border Protection officials who mistook her for actual human remains due to her lifelike appearance when she was shipped from overseas in a coffin-like pine box.
“You’ve got to love British humor,” said Click recalling the memory.
More than a spooky surprise
The school’s simulation center is home to a variety of manikins that enable students to gain hands-on experience in a risk-free environment. Low-, mid- and high-fidelity simulators can replicate scenarios from routine check-ups to critical emergencies, allowing students to practice their skills before interacting with live patients.

“We have simulators that breathe, bleed and even deliver babies,” Click explained.
One of the most popular simulators, Victoria, allows students to assist her in childbirth. She provides them, male students in particular, the opportunity to experience something they otherwise might miss out on due to cultural or privacy concerns.
“It’s not common that you can have a real patient deliver on demand,” said Click. “Victoria can deliver her baby in under 10 minutes.”
She’s not the only star of the center. Its inventory features a range of simulators, including pediatric and geriatric manikins, each designed to help students master different aspects of patient care.
Miss Vivian, the geriatric manikin who startled customs officials, is a particularly important teaching tool.
“She’s so lifelike that our vein finder can detect her veins, allowing students to practice starting IVs,” Click said.
A sophisticated learning environment
Nursing education goes beyond access to lifelike manikins; it’s about creating an immersive environment where students can hone their skills with the latest technology. Not long ago, the center added virtual reality (VR) training to its repertoire, enabling students to practice interacting with virtual patients before moving on to the manikins.

“Students wear VR headsets and walk through a patient scenario, interacting with both the patient and family members,” said Click.
This helps them prepare for the emotional and technical aspects of patient care, including how to communicate with family members in stressful situations.
Once students complete the VR scenario, they transition to the physical manikins, where they perform hands-on tasks like changing wound dressings or administering medication. This multi-stage approach ensures that students are thoroughly prepared for real-world nursing situations. The simulators can even be programmed to respond to different medications, allowing students to see the effects of their interventions in real time.
“A nurse can do everything perfectly, the same way they’ve done it multiple times and all of a sudden, a patient responds differently. We want to see how they react,” Click said. “Do they call a doctor; do they try something else? We have to practice that.”
The school also conducts special simulations, such as The Virtual Dementia Tour, which offers students and caregivers the opportunity to live with dementia for eight minutes. Participants’ senses are temporarily impaired while they are instructed to complete a series of tasks.

“They are only given the instructions once,” Click said. “We sometimes have participants who come out of the simulation feeling guilty for how they might have treated a loved one. It’s not until you experience similar symptoms do you really understand how debilitating dementia can be.”
The school also runs the Hearing Voices Simulation, demonstrating schizophrenia. It’s an eye-opening experience according to Braulio Amezaga, the lab’s manager of audio visual and teaching support services.
“Participants are given a list of tasks to complete in different areas of the school,” Amezaga said. “They must try to complete them while wearing headphones the entire time. The sound coming from the headphones simulates the voices someone with schizophrenia might experience.”
Amezaga said the voice starts off by softly humming but vastly changes by the end of the simulation.
“We warn participants that the voice becomes quite rude,” he said. “The simulation was created by Dr. Patricia E. Deegan, a researcher and educator in mental health recovery who was diagnosed with schizophrenia as a teenager, so it’s very realistic and participants find it extremely hard to concentrate.”
A glimpse of the future
As health care technology continues to advance, the Center for Simulation Innovation remains committed to staying on the cutting edge.
“We are always looking for new ways to improve the learning experience for our students,” said Amezaga, who mentioned that the school is preparing to add artificial intelligence (AI) to its tool belt.
A special smart speaker will soon allow the school to use conversational AI, permitting students to practice patient communication skills across several scenarios. The system will offer real-time feedback on communication effectiveness and includes preloaded scenarios such as abdominal pain, chest pain and allergic reactions.
“We’ll be able to program medical history and a personality to our manikins,” Amezaga said. “When students interact within a simulation, the AI can take over and respond randomly. It will make the scenarios that much more lifelike.”
Whether it’s through AI, VR, advanced simulators or even innovative moulage techniques that replicate real wounds, the center provides a comprehensive and immersive learning environment.
Distinctive in South Texas
While spooky tales of manikins coming to life after hours may circulate, it’s important to remember that behind the fun tales lies a serious mission: preparing the next generation of nurses with the skills and confidence to provide exceptional patient care.
In the fall of 2023, the Center for Simulation Innovation earned accreditation from the Society for Simulation in Healthcare for excellence in teaching and education. The recognition places it among the top simulation centers statewide and highlights its role in preparing nursing and inter-professional teams for clinical practice.
The accreditation process took two years and validates the center’s high standards in delivering simulation-based education.
“Our goal is to ensure that when our students graduate, they are practice-ready and confident in their abilities,” said Click. “The technology we have allows them to experience situations they might not encounter in their clinical rotations — they’ll be ready for anything.”
Hormone fluctuation and women’s oral health
Hormones. These chemical messengers hold the power to regulate mood, energy levels, sleep, appetite and libido — but changes in oral health, too?

“It’s true,” exclaimed Maiara Hister-Cockrell, DDS, an associate professor/clinical at The University of Texas Health Science Center at San Antonio School of Dentistry. “From puberty to menopause, a woman’s entire body, including [her] mouth, is impacted by the rise and fall of hormones,” she said.
The surge of growth and reproductive hormones that accompany certain life stages increase the flow of blood to multiple body sites including the gums. Hister-Cockrell said this increase of blood, estrogen and progesterone alters the response of gum tissue to bacteria that accumulate around teeth and under the gumline.
Later in life, when hormone levels fall significantly, it can affect saliva production, bone density, such as that of the jaw, or contribute to burning sensations in the mouth.
Navigating adolescence
“Let’s think about puberty,” Hister-Cockrell said. “The increase in hormones triggers puberty and also swells the gums, making them sensitive. They are easily irritated and prone to bleeding.”
While the gums are vulnerable, they are subject to infection by bacteria that live naturally in the mouth. Hister-Cockrell said a diligent oral hygiene routine is important to prevent early-stage gum disease known as gingivitis.
“Allowing bacteria to colonize around the teeth can lead to gingivitis and gingivitis can lead to periodontitis, tooth decay and worse, so it’s important to brush and floss every day to prevent this,” she said.
 The same surge of hormones and gum sensitivity occurs a few days before a menstrual period, Hister-Cockrell said. Canker sores are likely to appear as well but should quickly heal on their own once bleeding stops. Any noticeable swelling or sores in the mouth that do not subside afterward should be examined by a dentist.
The same surge of hormones and gum sensitivity occurs a few days before a menstrual period, Hister-Cockrell said. Canker sores are likely to appear as well but should quickly heal on their own once bleeding stops. Any noticeable swelling or sores in the mouth that do not subside afterward should be examined by a dentist.
Hister-Cockrell added that adolescence is a challenging life stage for dental health due to the social changes that occur alongside the physical ones.
“Parents have more control of what small children eat,” she said. “Teens and preteens are more exposed to carbonated drinks and fast food. It’s also during this stage that parents stop closely supervising nightly hygiene routines since they are considered old enough to manage on their own. But they are still developing, so more often than not, they don’t brush well enough or sometimes at all. This combination is not favorable for their teeth.”
Impacts of birth control and pregnancy
Individuals on birth control or who are pregnant find themselves on two sides of the same coin. For both, Hister-Cockrell said hormone levels look similar.
“Just like women who are pregnant, women who take contraceptives must watch their oral health,” she said. “This is because contraceptives mimic the state of pregnancy, so you have higher levels of progesterone and estrogen. This surge again makes women vulnerable to bacteria colonization and gingivitis.”
A hormonal contraceptive, such as the birth control pill, can also disrupt the healing process after a dental procedure depending on estrogen and progesterone levels. In a procedure such as a tooth extraction, a person on hormonal contraception is twice as likely to develop a painful condition called a dry socket. Most dentists suggest people on birth control schedule such a procedure during the last week of their menstrual cycle or during the “sugar pill” days when hormone levels are lowest.
 An expectant parent faces even greater oral health stress. Gingivitis is seen in 60% to 75% of pregnant individuals, suggesting that pregnancy is one of the roughest life stages for oral health. What’s worse, Hister-Cockrell said, is that many people stop seeing a dentist during their pregnancy.
An expectant parent faces even greater oral health stress. Gingivitis is seen in 60% to 75% of pregnant individuals, suggesting that pregnancy is one of the roughest life stages for oral health. What’s worse, Hister-Cockrell said, is that many people stop seeing a dentist during their pregnancy.
“Visualize it. You’re growing a baby, right? You’re seeing a doctor already. You’re uncomfortable and can’t sit for long, but it’s so important,” she said. “Some people even believe seeing a dentist while pregnant will hurt their baby, but gestational gingivitis is real.”
Seeing a dentist during the second trimester of pregnancy is vital for more than gum health, Hister-Cockrell said. The overall health of both parent and child could depend on it.
“Periodontal or gum disease is linked to preterm delivery and infants with low birth weight,” she said. And according to Hister-Cockrell’s review of the literature, “even preeclampsia can be associated with it.”
Pregnant individuals with gum infections are at 7.5 times higher risk for preterm delivery of low-birth-weight infants than those without infections. This is because the bacteria infecting the parent’s gums can travel through the bloodstream and pass through the placenta to the unborn child. Depending on when this occurs, the severity of the infection and the stage of the baby’s development, the consequences could range from low birth weight to miscarriage.
“The good thing is that this is all preventable under a dentist’s care,” Hister-Cockrell said.
Both the American Dental Association and The American College of Obstetricians and Gynecologists have stated that seeing a dentist during pregnancy is safe.
Vigilance during menopause
What remains unavoidable, despite recent advancements, is aging. Menopause typically occurs when women reach their 40s or 50s, a time when their ovaries significantly reduce the production of reproductive hormones. However, it can occur earlier due to a family history of premature menopause or other medical conditions.
As estrogen and progesterone decrease, a number of changes occur in the body. Menstruation becomes irregular and then stops, body temperature fluctuates and hair growth and sleep cycles change, but two changes in particular significantly affect a woman’s oral health, Hister-Cockrell said. Bone loss and dry mouth are common among menopausal women.
 “When you hear conversations about menopause, you usually hear discussion of osteoporosis,” she said. “This is because bone density decreases with the lower hormone levels and continues to do so after menopause.” Studies show that on average, women lose up to 10% of their bone mass in the first five years after menopause.
“When you hear conversations about menopause, you usually hear discussion of osteoporosis,” she said. “This is because bone density decreases with the lower hormone levels and continues to do so after menopause.” Studies show that on average, women lose up to 10% of their bone mass in the first five years after menopause.
“Why is this important for oral health? Because bone is part of a structure that holds our teeth in place,” Hister-Cockrell said. “If we start to lose the bone around our teeth, our gums may recede, the roots of our teeth stand to be exposed making them sensitive and unstable, prone to further bone and gum loss. Some people may notice that with age, their teeth begin to shift, this may be because of bone loss around the teeth making them less solid than when they were 20 years old.”
Dry mouth and burning mouth syndrome are also symptoms Hister-Cockrell sees in clinical patients at this life stage.
“Salivary glands are known to decrease their production of saliva in some women during menopause. This makes the mouth feel dry and can make chewing, swallowing and speaking difficult. Certain medications can also cause dry mouth,” she said.
She added that saliva is an important component to maintaining oral health, so its reduction needs to be monitored.
“Saliva helps to protect against tooth decay and infection due to its pH level,” she said. By helping to neutralize the pH in the mouth after eating or drinking, saliva defends against an acidic environment that would promote the breeding of harmful bacteria.
A burning or scalding sensation, known as burning mouth syndrome, can sometimes be linked to dry mouth. “It can come on quickly or over time and can cause tingling or numbness and change taste or bring on a metallic taste,” Hister-Cockrell said.
‘Dental care is health care’
At any life stage, Hister-Cockrell advises regular dental visits and a strong dental hygiene routine to maintain oral health.
“A dentist will help to identify an effective treatment plan for any of these conditions and can help a primary care doctor monitor a woman’s overall health. After all, the mouth is part of our body — dental care is health care,” she said.
Studying the impact of antibiotics in dental care
Periodontal disease affects nearly 40% of the U.S. Periodontitis, or severe gum disease, is one of the most common inflammatory diseases in adults worldwide. It can be difficult to manage, often resurging despite treatment and triggering tooth loss, jawbone damage and a constant, low-level inflammation that increases the risk of systemic inflammatory illnesses such as diabetes or cardiovascular disease.
In tandem with a deep cleaning, dentists often prescribe antibiotics to combat inflammation of the gums caused by bacteria in plaque. Researchers and practitioners want to better understand which patients positively respond to antibiotics.
With a four-year, $2.4 million grant from the National Institutes of Health, School of Dentistry researchers will work in collaboration with the American Dental Association Science & Research Institute to conduct a clinical trial studying the responsible use of antibiotics in combination with other treatments for periodontal disease.
The study, funded by NIH’s National Institute of Dental & Craniofacial Research, is led by principal grant recipient and investigator Georgios Kotsakis, DDS, MS, associate professor of periodontics. The institute’s chief executive officer Marcelo Araujo, DDS, PhD, serves as co-investigator and collaborator. It is one of the largest dental clinical trials in the U.S., Kotsakis said.
Kotsakis and his team in the Translational Periodontal Research Lab will generate data from 1,050 periodontal patients treated with antibiotics. More than 30 clinicians nationwide, belonging to the National Dental Practice- Based Research Network, will share patient outcomes and experiences, contributing data to the development of evidence-based clinical guidelines, treatment alternatives and information on proper antibiotic use.
“With the current rise of superbugs, which are bacteria that kill tens of thousands of Americans every year due to antibiotic resistance, there is a critical need to determine if specific patient populations benefit from adjunctive antibiotics,” Kotsakis said.
The new trial is expected to begin in spring 2023, and the periodontal patients will be treated and followed over a period of approximately one year.






