After 61-year-old Bobbie Thompson had an ischemic stroke, her face drooped. She couldn’t lift her left arm. Her carotid artery carrying oxygen-rich blood to her brain was blocked.
Without immediate intervention, her brain tissue would begin to die.
Each year, nearly 800,000 people in the U.S. have a stroke. About 87 percent of the time, the cause is a clot that blocks an artery and restricts blood flow to the brain, called an ischemic stroke. Because brain tissue begins to die, opening the artery quickly is essential.
For 20 years, physicians have used the clot-busting medication called intravenous tPA, but often it doesn’t help patients, like Thompson, whose largest vessels are blocked. They are now pairing emergency interventional procedures to open the vessel, save brain tissue and preserve quality of life.
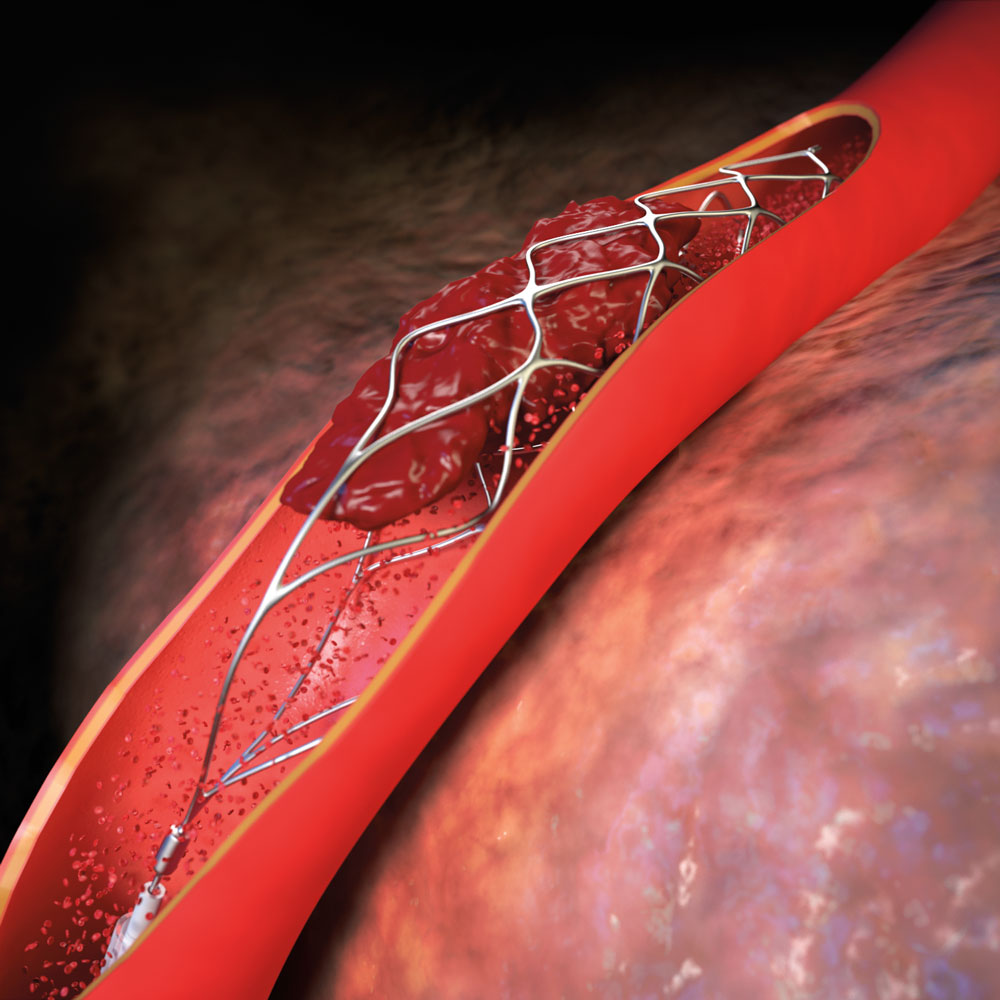
Using devices called “stent retrievers,” they extract clots from stroke patients with large-vessel blockages. Stent retrievers, about the size of a coffee stir, are attached to a catheter that is threaded from the groin to the brain’s largest vessels. The stent is used to open a hole through the clot and reestablish blood flow. The stent attaches to the blood clot and is then pulled back down the vessel toward the groin and removed from the body.
Restoring blood flow as quickly as possible is important in most stroke patients with large-vessel blockages who are transported to the hospital early, said neurosurgeon Ramesh Grandhi, M.D., assistant professor in the Department of Neurosurgery.
“Amongst those patients, CT imaging shows that a large portion of the brain is at risk of dying from a blood vessel blockage but is not yet dead,” Dr. Grandhi said. “If circulation resumes quickly enough, the at-risk brain survives.”
In cases such as Thompson’s, intravenous tPA may not work by itself. The resulting stroke can cause patients to lose so much function that they require around-the-clock nursing home care.
But with the help of stent retrievers, a full recovery is possible. Two days after her stroke, Thompson had no residual paralysis. Today, she smiles fully, can move both arms freely, and walks around without a limp.
“Her arm would never have moved again, but here she is giving a thumbs-up to her doctors,” said neurosurgeon Jeremiah Johnson, M.D., of UT Medicine. “Those are the kind of results we want for our stroke patients.”
The UT Medicine Comprehensive Stroke and Cerebrovascular Program includes four vascular neurologists, three neuro-interventional surgeons, a neuro-intensive care team, rehabilitation medicine specialists and additional neurosurgeons. The team operates at University Hospital and in the Baptist Health System.
“UT Medicine provides the community a comprehensive team of academic experts who are supported by our clinical partners,” said David F. Jimenez, M.D., FACS, professor and chairman of the Department of Neurosurgery. “From stroke to brain aneurysms to other conditions, there isn’t anything in the cerebrovascular world that we don’t do here.”
