UT Medicine surgeons revolutionize repair of unstable breastbones
Using a “mixed tool bag of techniques,” including a ratchet mechanism, UT Health San Antonio physicians in three disciplines — cardiothoracic surgery, radiology and plastic surgery — provide a new breakthrough for patients with unstable breastbones.
Leroy Lorenz’s breastbone failed to heal back together after a coronary artery bypass operation. Donna Lea Anderson’s breastbone was eaten away by a staph infection, a complication of aortic valve surgery. Both lived with chronic pain and disconcerting internal movement for months. Then they discovered an innovative breastbone reconstruction technique performed by specialists from UT Health Physicians. UT Medicine is the clinical practice of the Long School of Medicine at the UT Health Science Center.
Leroy Lorenz and Donna Lea Anderson are among the estimated 400,000 people a year who undergo surgery to bypass arteries, repair heart valves and correct other problems. These surgeries require dividing the breastbone, which afterward is commonly repaired with stainless steel wire. Healing is normal in most cases, but in up to 3 percent of patients (12,000 a year) the breastbone comes apart. Morbid obesity, poorly controlled diabetes, chronic coughing and vitamin D deficiency often related to osteoporosis increase the risk of this serious complication.
The breastbone, or sternum, anchors the rib cage protecting the heart and lungs. Cardiothoracic surgeons, plastic surgeons and radiologists from UT Medicine pioneered a corrective surgery that employs three technologies to help these patients.

 A year after his surgery, Leroy Lorenz’s reconstructed breastbone is strong enough to handle the jostling of mowing the family property on his new lawn tractor. He’s also trimming oak trees with a pole trimmer, picking up limbs and clearing fence line. It’s a newfound freedom, his wife says.
A year after his surgery, Leroy Lorenz’s reconstructed breastbone is strong enough to handle the jostling of mowing the family property on his new lawn tractor. He’s also trimming oak trees with a pole trimmer, picking up limbs and clearing fence line. It’s a newfound freedom, his wife says.
Cardiothoracic surgeons ensure the heart is not nicked, as its proximity to the breastbone is razor thin. , professor and chair of the Department of Cardiothoracic Surgery in the Long School of Medicine, leads members of a team that work on these high-risk cases. “It is usually quite uncomfortable for a person to not have a solid breastbone,” Dr. Calhoon said. “The grating movement of an incompletely healed sternum can cause chronic pain and lead to anxiety and depression. These patients are often led to believe nothing can be done.”
Cardiothoracic surgeons ensure the heart is not nicked, as its proximity to the breastbone is razor thin. , professor and chair of the Department of Cardiothoracic Surgery in the Long School of Medicine, leads members of a team that work on these high-risk cases. “It is usually quite uncomfortable for a person to not have a solid breastbone,” Dr. Calhoon said. “The grating movement of an incompletely healed sternum can cause chronic pain and lead to anxiety and depression. These patients are often led to believe nothing can be done.”
Cardiothoracic surgeons ensure the heart is not nicked, as its proximity to the breastbone is razor thin. John Calhoon M.D., professor and chair of the Department of Cardiothoracic Surgery in the Long School of Medicine, leads members of a team that work on these high-risk cases. “It is usually quite uncomfortable for a person to not have a solid breastbone,” Dr. Calhoon said. “The grating movement of an incompletely healed sternum can cause chronic pain and lead to anxiety and depression. These patients are often led to believe nothing can be done.”
Lorenz, a truck driver from Seguin, underwent reconstruction in May 2011 at CHRISTUS Santa Rosa Hospital – New Braunfels. His breastbone was divided in a bypass operation in 2009. After the surgery, when it was expected to have healed, he felt a gap inside and shared this with his wife, Leigh Ann. “You could actually put your hand on the bone and move it around and feel all my innards moving,” he said. A chest X-ray confirmed that the breastbone had separated and the wires were broken into several pieces.
Anderson, a writer/lyricist from San Antonio, underwent reconstruction in April 2011 at University Hospital in San Antonio. A staph infection destroyed her sternum after her second heart valve operation, causing the top four-fifths of the sternum to be removed. “For a year and a half, my ribs rubbed together and I heard popping whenever I moved,” she said.
How the surgery is done
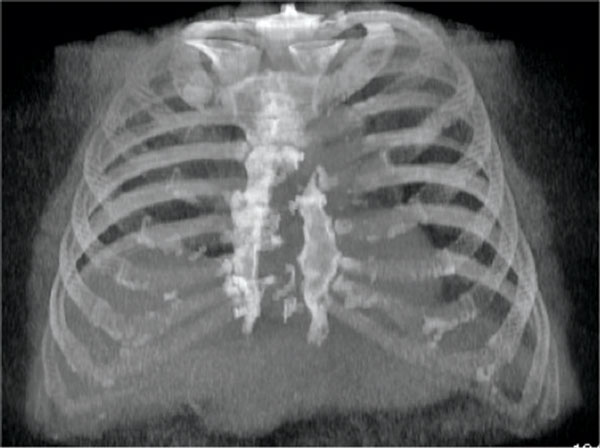
Carlos Restrepo, M.D., a chest radiologist with UT Medicine, uses advanced CT imaging to confirm the separation of the sternum. Because every patient is different, it is important to visualize the exact anatomic details surgery will correct. “CT images also show infection, if it is present, which is a common explanation for why the surgical wound is opening instead of healing,” Dr. Restrepo said.

 In surgeries such as artery bypass and heart valve repair, the breastbone is divided and afterward is commonly repaired with stainless steel wire (top). In a small percentage of cases, the breastbone comes apart and the wires can break. UT Health San Antonio physicians are using several techniques, including Sternal Talons® illustrated above, to fix the breastbone in place and correct the problem.
In surgeries such as artery bypass and heart valve repair, the breastbone is divided and afterward is commonly repaired with stainless steel wire (top). In a small percentage of cases, the breastbone comes apart and the wires can break. UT Health San Antonio physicians are using several techniques, including Sternal Talons® illustrated above, to fix the breastbone in place and correct the problem.
Aided by digital imaging, a cardiothoracic surgeon lifts the sternum off the heart and removes scar tissue on it. A UT Medicine plastic surgeon on the case, either Howard Wang, M.D., or Luis Jaramillo, M.D., dissects muscle away from the breastbone. With the breastbone exposed, the cardiothoracic surgical team reassembles the pieces like a puzzle, using a mixed “tool bag of techniques” sometimes including Sternal Talons® to fix the breastbone in place. A ratchet mechanism is used to pull the sides together.
The cardiothoracic surgeon may also utilize orthopedic plating techniques to stabilize the sternum. Because the two sides of the fracture are jagged and leave gaps when drawn tight, the surgeon may also employ Kryptonite™ Bone Cement, which provides a bridge for bone cells to migrate across, filling the gaps. Full healing can then take place.
Afterward, a plastic surgeon inserts muscle or fat from the chest or other parts of the body to fill the chest space with strong tissue that brings good circulation. This provides protection, blood supply, healing and the ability to deliver antibiotics. “Bone, tendon and vital organs must be covered quickly to prevent dangerous infection,” Dr. Wang said.
Preventing problems
For high-risk patients such as diabetics who undergo chest surgery, a number of sternal closure methods such as those described above may be considered. “At the end of the day, what matters most is creating a solid breastbone again as safely as possible,” Dr. Calhoon said.
“I put up with it (the unnatural feeling in his chest) for a year and a half, but since the operation I’ve been able to do more stuff around home than I have the last two years,” Lorenz said.
Anderson’s surgery also involved implantation of synthetic bone to replace the large amount of sternum that deteriorated by infection. “I can move now without hearing the snap, crackle and pop,” Anderson said. “I know my sternum is stabilized and mentally that does so much for me.”
For information about this type of surgery, call UT Health San Antonio Cardiothoracic Surgery at 210-358-8001 or visit UTHealthPhysicians.org
